Post LVAD Management
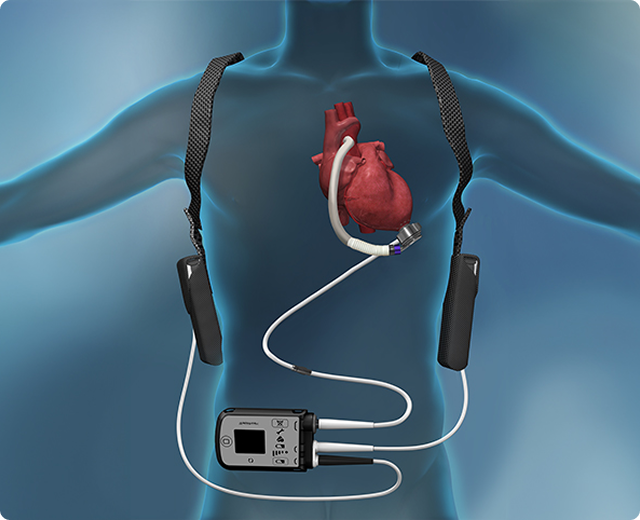
Following a left ventricular assist device (LVAD) procedure, patients enter a critical recovery phase in the ICU, where continuous LVAD patient monitoring ensures stability. The Save Heart Failure initiative employs advanced hemodynamic monitoring systems and INTERMACS profiling to assess patient progress. Anticoagulation therapy with blood-thinning medications like warfarin prevents clot formation, while specialized LVAD driveline care minimizes infection risks. Our dedicated cardiac rehabilitation team provides customized low-impact exercise plans and psychosocial support, promoting holistic recovery. With state-of-the-art remote monitoring systems, patients receive real-time care adjustments. Long-term follow-ups ensure mechanical circulatory support function and heart health optimization under Dr. Merchant’s expert supervision.
What Happens After a Left Ventricular Assist Device Procedure?
Recovery in ICU

Patients undergo intensive care monitoring in the ICU using invasive hemodynamic monitoring devices to track LVAD flow and detect early heart failure complications.
Hospital Stay & Monitoring

Patients transition to a step-down care unit, receiving daily assessments using echocardiography, blood tests, and cardiac telemetry to fine-tune their recovery.
Blood Thinner Medications

Anticoagulation therapy with warfarin and regular INR monitoring prevents clot formation, reducing stroke risk and ensuring safe blood thinning medication levels.
Wound Care & Healing

Strict aseptic dressing protocols and infection prevention strategies are employed. Our nursing staff provides wound care education for continued home management of driveline site infections.
Cardiac Rehabilitation & Lifestyle Adjustments

Supervised cardiac rehab post-LVAD includes tailored low-impact exercises and dietary guidance, with psychological support to enhance mental well-being and LVAD lifestyle adjustments.
Long-Term Follow-Up

Regular follow-ups feature device performance evaluations using remote monitoring tools. Adjustments to medication management and lifestyle plans ensure sustained recovery.
Risks and Complications After an LVAD Procedure
While LVADs improve survival and quality of life, potential complications include bleeding complications, infection, and stroke risk with LVAD. Device malfunction and pump thrombosis are closely monitored using advanced diagnostics. Right heart failure remains a concern, particularly in INTERMACS Profile 1 patients, requiring additional therapies like inotropes or RVAD support. Through proactive risk management, personalized anticoagulation therapy, and frequent follow-ups, Dr. Merchant’s heart failure team minimizes these risks and ensures prompt intervention when necessary.
Long-Term Outlook and When to Consider Heart Transplant
Signs That a Heart Transplant May Be Needed
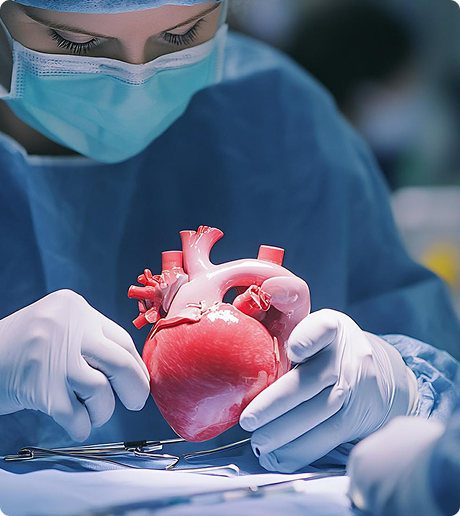
Persistent INTERMACS Profile 4-7 symptoms, refractory heart failure despite LVAD support, or end-organ dysfunction may necessitate heart transplant evaluation.
Eligibility for a Heart Transplant
Eligibility is assessed through comprehensive evaluations, including cardiopulmonary testing, organ compatibility, and psychosocial assessments.
Advances in Heart Failure Treatment
Cutting-edge innovations such as magnetically levitated LVADs, gene therapy, and regenerative medicine offer improved heart failure management options.
Appointments Will I Need?
book an Appointment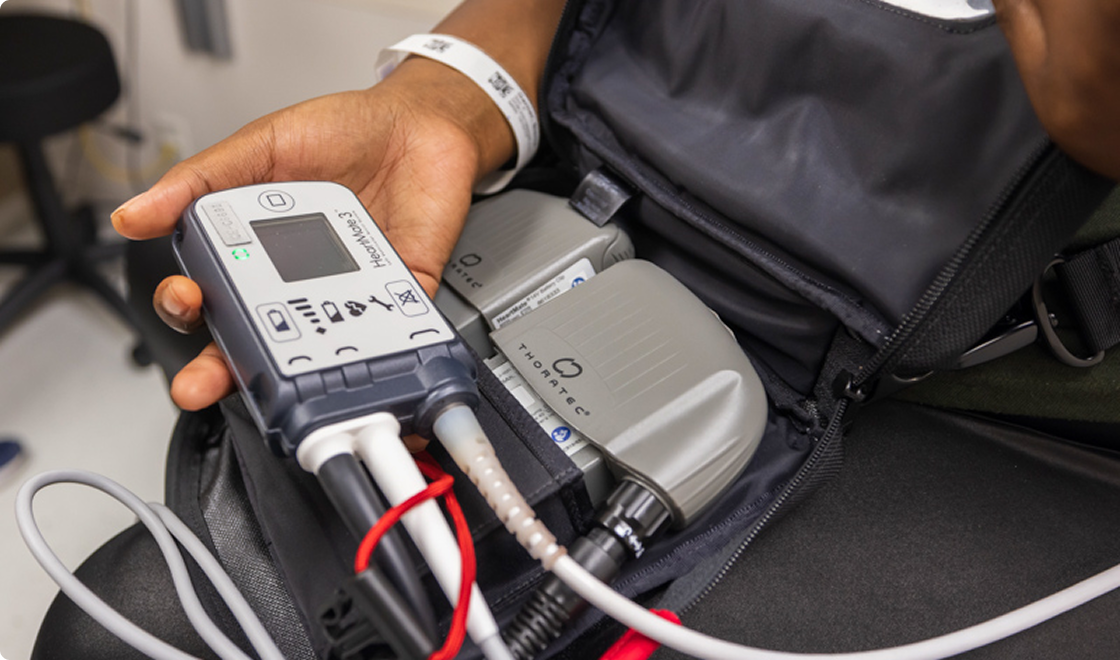
Patients undergo routine device interrogation using remote monitoring systems, ensuring early detection of potential LVAD malfunctions.

Frequent blood tests, including INR monitoring, ensure optimal anticoagulation therapy tailored to minimize bleeding and clotting risks.

Scheduled wound assessments are conducted using infection risk algorithms to guide preventive care and early intervention if needed.

Holistic follow-ups evaluate exercise capacity using cardiopulmonary testing, with nutritional support and mental health support integrated into the recovery plan.
frequently asked questions
-
Yes, medications like beta-blockers and ACE inhibitors can manage symptoms, improve heart function, and prevent further progression.
-
While heart failure can’t always be cured, treatments like heart transplants or LVADs offer long-term management and improved quality of life.
-
High blood pressure forces the heart to work harder, weakening it over time and increasing the risk of heart failure.
-
Heart failure is more common in people over 65, but it can occur at any age, especially with risk factors like hypertension or heart disease.
-
A heart failure patient’s target blood pressure is typically around 120/80 mmHg, but doctors may adjust goals based on individual conditions.
