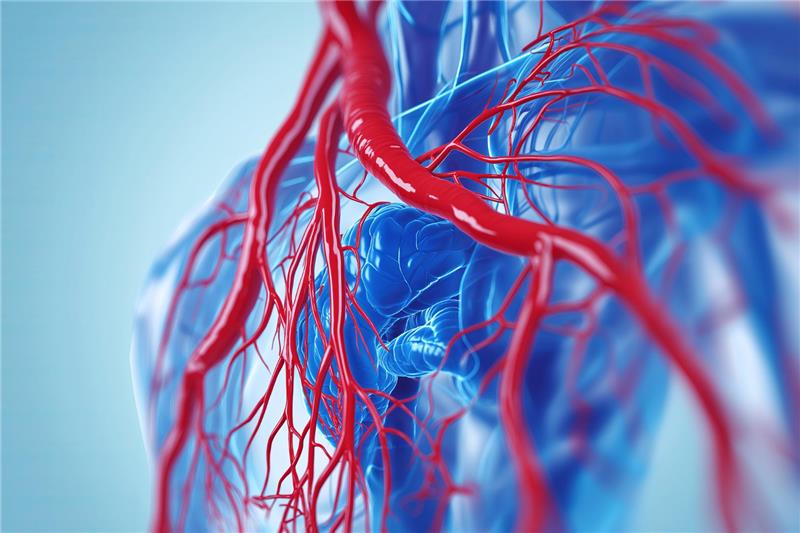
Heart failure affects millions globally and is a progressive condition in which the heart is unable to pump enough blood to meet the body’s needs. Traditional treatments often involve medications and, in advanced stages, open-heart surgeries. However, advances in cardiovascular medicine have introduced minimally invasive procedures as safer and more effective alternatives for select patients. These approaches are revolutionizing how heart failure is managed, offering faster recovery times and fewer complications compared to conventional surgery.
What Makes a Procedure Minimally Invasive?
A minimally invasive procedure involves the use of smaller incisions, specialized instruments, and advanced imaging to treat or manage heart conditions. Unlike open-heart surgery, which requires a large chest incision and stopping the heart temporarily, minimally invasive techniques aim to achieve similar results with reduced physical trauma. These procedures often use catheter-based techniques or small incisions between the ribs, allowing the heart to be treated while it continues to function.
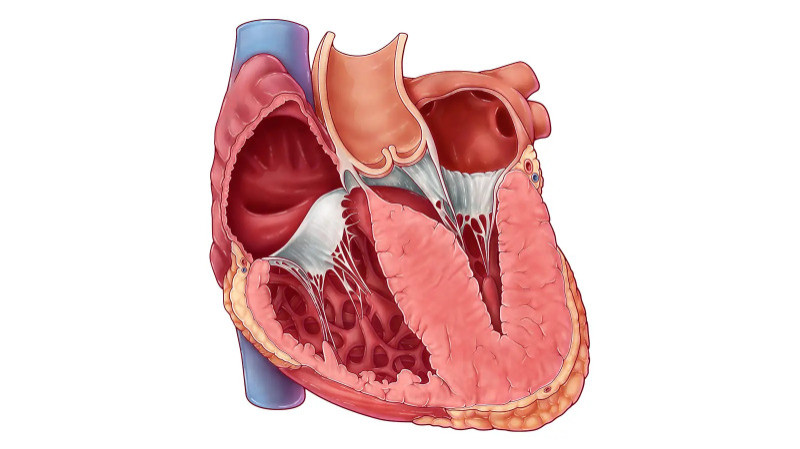
Transcatheter Mitral Valve Repair and Replacement
In many heart failure patients, the mitral valve does not close properly, leading to a condition known as mitral regurgitation. This can worsen symptoms and strain the heart over time. Transcatheter mitral valve repair or replacement allows doctors to correct the problem without opening the chest. Through a catheter inserted via the groin or chest, a clip or new valve is guided into the heart and positioned to improve valve function. This procedure has shown significant improvement in heart failure symptoms and quality of life.
Minimally Invasive Coronary Artery Bypass Surgery
Patients with heart failure often have blocked coronary arteries. Traditionally, bypass surgery involves a long recovery due to a large incision in the chest. Minimally invasive coronary artery bypass can be performed through small incisions, sometimes using robotic assistance. This allows surgeons to bypass blocked arteries and restore blood flow with less postoperative pain and a quicker return to normal activities.
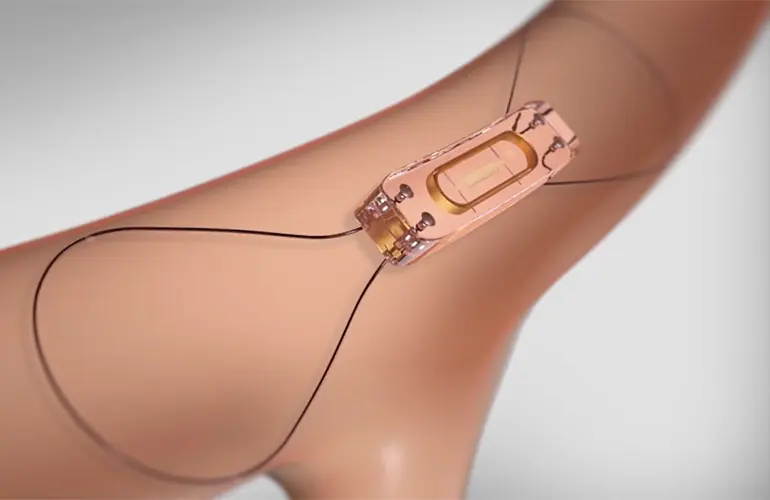
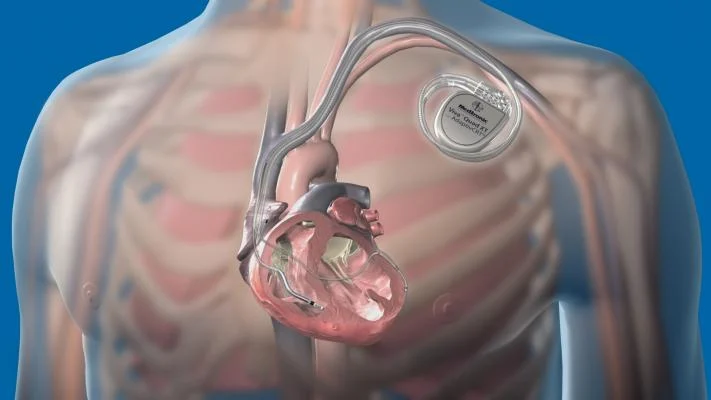
Implantation of Cardiac Devices through Catheter Techniques
Devices like pacemakers and implantable cardioverter-defibrillators (ICDs) are vital for managing rhythm-related heart failure issues. Minimally invasive implantation of these devices involves inserting leads and the device itself through small incisions, typically in the chest or neck. Advanced imaging techniques help ensure precise placement. Newer technologies allow for leadless pacemakers and subcutaneous ICDs, further reducing surgical complexity and infection risk.
Transcatheter Aortic Valve Implantation (TAVI)
TAVI is a major breakthrough for patients with severe aortic stenosis who are at high risk for open surgery. In heart failure patients, this condition can further weaken the heart. TAVI involves threading a new valve into the heart via a catheter, often through the femoral artery. Once positioned inside the damaged valve, the new valve expands and begins functioning immediately. This approach has made life-saving valve replacement possible for many patients who were previously considered inoperable.
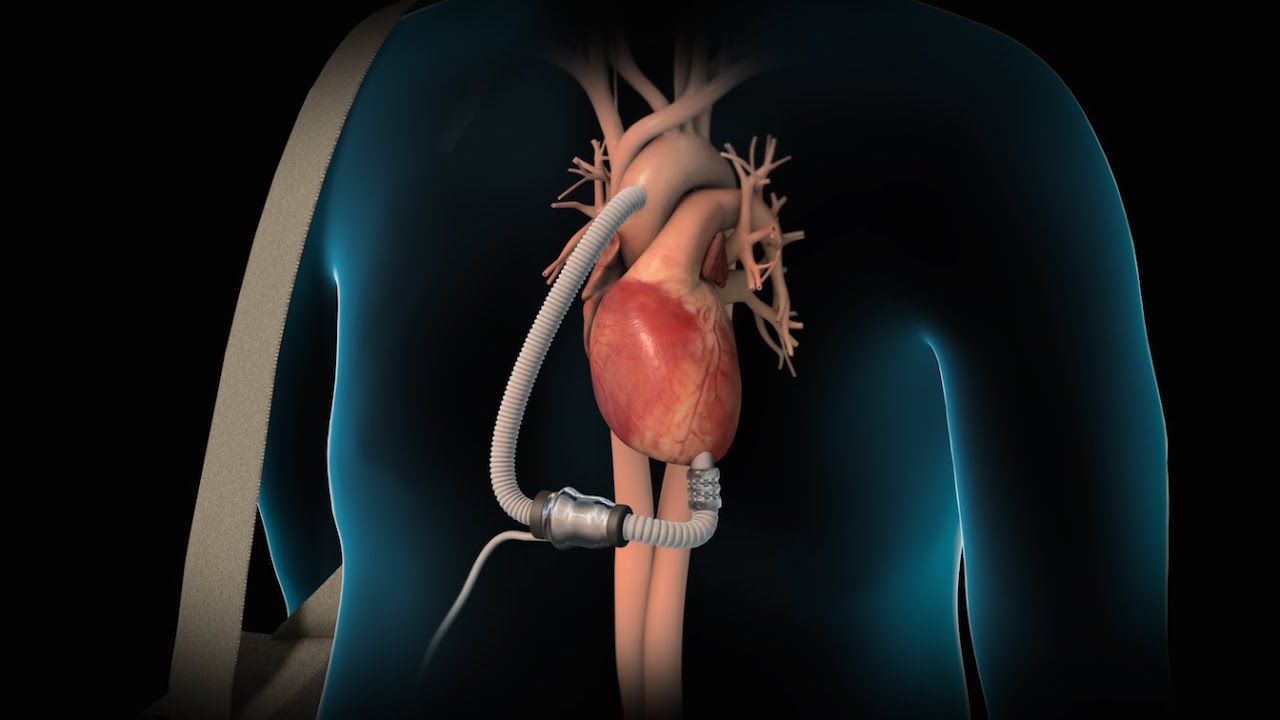
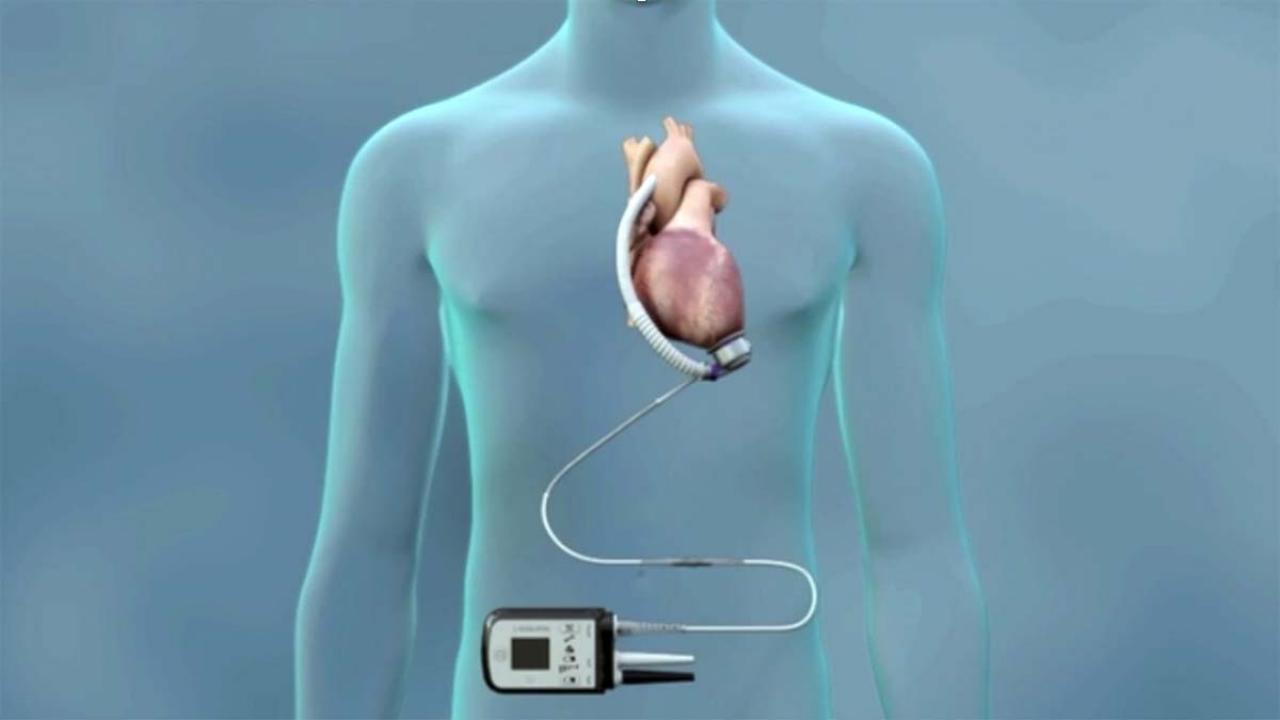
Left Ventricular Assist Device (LVAD) Implantation via Minimally Invasive Access
LVADs are mechanical pumps that support heart function in advanced heart failure. Recent innovations have enabled the implantation of these devices through less invasive techniques. Smaller chest incisions, avoiding the need to open the breastbone, have led to shorter hospital stays and reduced recovery times. This advancement has broadened the eligibility for LVAD support among patients who may not tolerate conventional surgery.
Benefits of Minimally Invasive Treatments for Heart Failure
Patients undergoing minimally invasive procedures generally experience less pain, lower risk of infection, and faster recovery. These methods reduce hospital stays and often allow quicker return to daily activities. For elderly patients or those with multiple health conditions, these procedures present safer alternatives to traditional surgery. Importantly, they provide effective symptom relief and help prevent further heart damage.
Expanding Accessibility and Future Outlook
Ongoing research and development are expanding the availability of minimally invasive techniques to more heart failure patients. Innovations in robotics, imaging, and device design are making procedures more accurate and personalized. As awareness grows and technology advances, these methods will likely become standard options for managing various stages of heart failure.
Conclusion
Minimally invasive procedures have transformed the treatment of heart failure, offering patients new hope with fewer risks and quicker recovery. From valve repairs to device implants, these techniques are proving to be life-enhancing alternatives to traditional surgery. As technology continues to evolve, the role of minimally invasive interventions will become even more central in the comprehensive care of heart failure patients, leading to better outcomes and improved quality of life.