Advanced heart failure represents the most critical stage of heart dysfunction, where the heart’s pumping ability becomes severely impaired. Patients often experience persistent symptoms such as breathlessness, fatigue, fluid retention, and reduced exercise capacity, even with maximum medication. At this point, conventional therapies fail to provide sufficient relief, and mechanical support systems like ventricular assist devices (VADs) become a potential solution.
Defining a Ventricular Assist Device
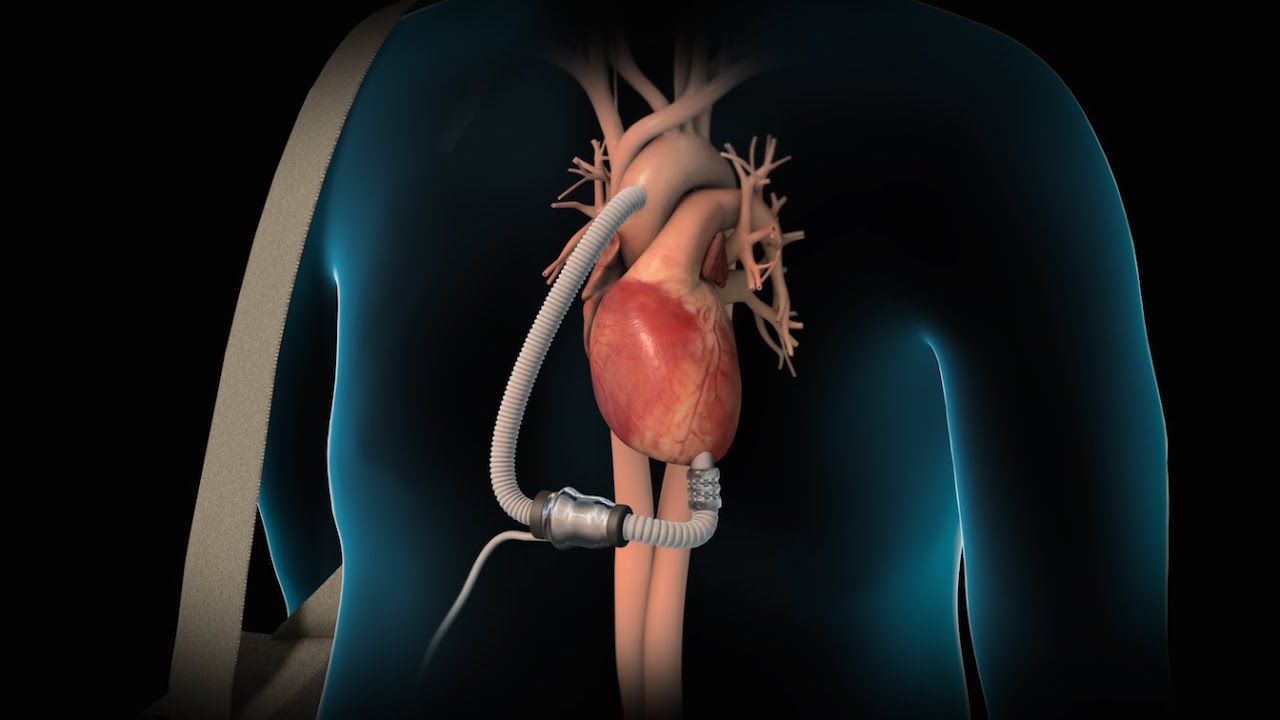
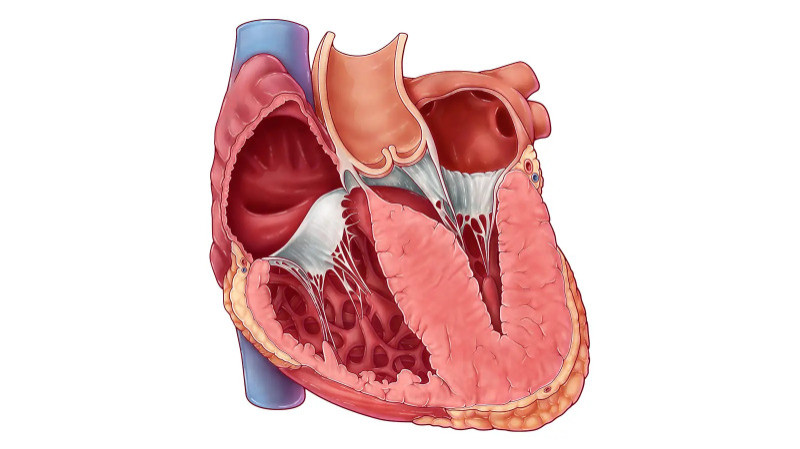
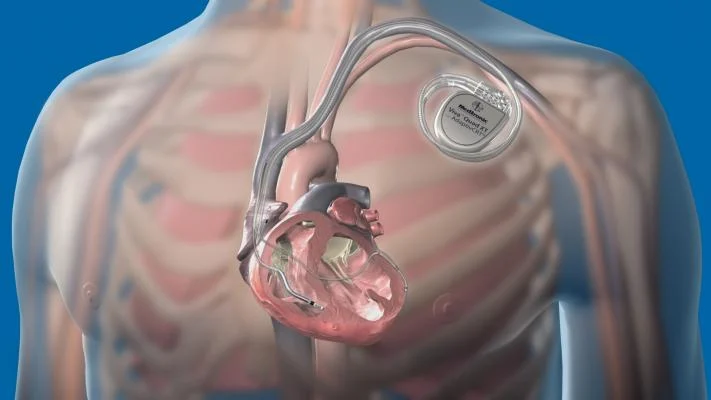
A ventricular assist device is a mechanical pump that helps the heart circulate blood more effectively. Most commonly, it assists the left ventricle—the heart’s main pumping chamber—and is referred to as an LVAD. However, depending on the patient's condition, a VAD can also support the right ventricle (RVAD) or both ventricles (BiVAD). These devices take over the pumping function of a failing heart, either temporarily or permanently, depending on the treatment goal.
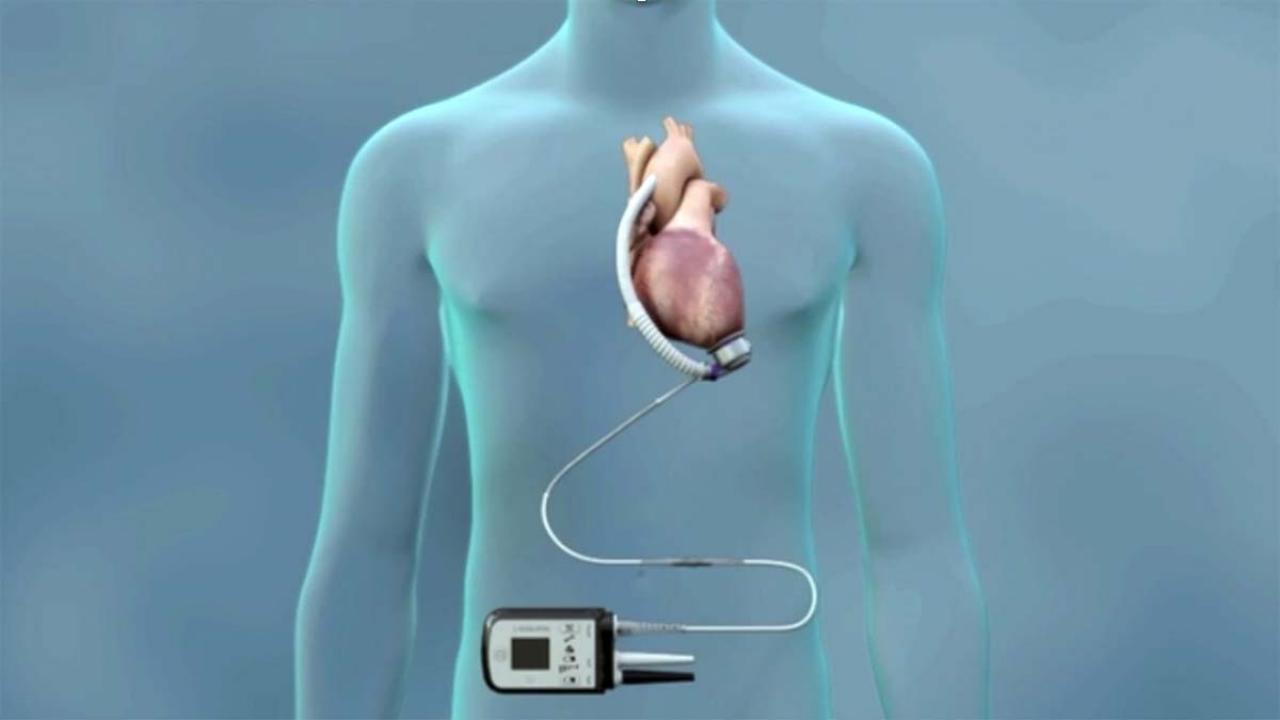
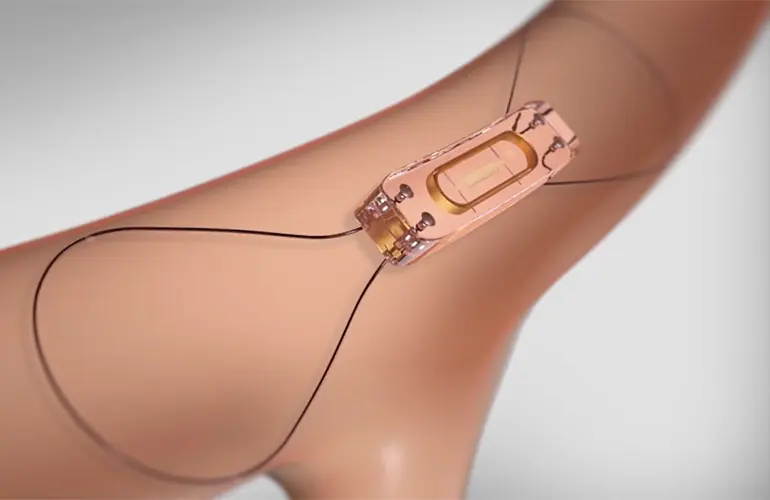
VADs are surgically implanted inside the chest and connected to a power source that remains outside the body. The system includes a controller and batteries that the patient carries externally, enabling long-term mobility and functionality.
Why Are VADs Used?
VADs were initially developed as a bridge to heart transplantation, allowing patients to survive until a donor heart becomes available. Over time, their application has expanded to include destination therapy for patients who are not candidates for transplantation. In some cases, VADs are used as a bridge to recovery, helping the heart heal from temporary damage.
By supporting cardiac output, VADs improve blood flow to vital organs, reduce symptoms, and often enhance the overall quality of life. Many patients report increased energy, improved breathing, and the ability to resume daily activities that were previously limited by their condition.
Surgical Procedure and Recovery
Implantation of a VAD requires major surgery, typically performed under general anesthesia in a cardiac center. After the device is implanted, patients spend time in intensive care for close monitoring. Recovery involves gradual rehabilitation, patient education, and adjustment to life with the device.
Learning to manage the external components, maintaining hygiene around the driveline site, and adhering to medication schedules are essential parts of the recovery process. Ongoing follow-up ensures that the device functions well and complications are minimized.
Living with a VAD
Adapting to life with a VAD is both a physical and emotional journey. Patients must adjust to carrying the external power unit and managing the device daily. Education and support are critical, and many hospitals provide specialized VAD coordinators to assist patients and families.
Despite the challenges, many people regain their independence and lead fulfilling lives. Activities like walking, light exercise, and even travel become possible again with proper planning and care.
Potential Risks and Challenges
Although VADs offer life-saving support, they are not without risks. Possible complications include bleeding, infection at the driveline site, device malfunction, and stroke. Anticoagulation therapy is often necessary to prevent blood clots, which requires regular monitoring.
Emotional health is also a key consideration. Patients may experience anxiety or fear related to the device, and counseling services are often recommended as part of comprehensive care.
Evolving Technology and Hope for the Future
VAD technology continues to improve rapidly. Modern devices are smaller, quieter, and more efficient than earlier models. Battery life has extended, and newer designs offer increased comfort and mobility. These advancements are making VAD therapy accessible to a broader range of patients.
Ongoing research is focused on fully implantable devices and artificial hearts, which could further revolutionize care for patients with end-stage heart failure.
Conclusion
Ventricular assist devices have become a crucial treatment option for individuals with advanced heart failure who no longer respond to traditional therapies. They restore blood flow, relieve symptoms, and often extend life while improving quality of life. As technology advances, VADs represent not just a bridge to transplant or recovery, but a reliable destination therapy in their own right. With skilled medical care, proper management, and patient education, VADs truly serve as a lifeline in the journey of heart failure treatment.