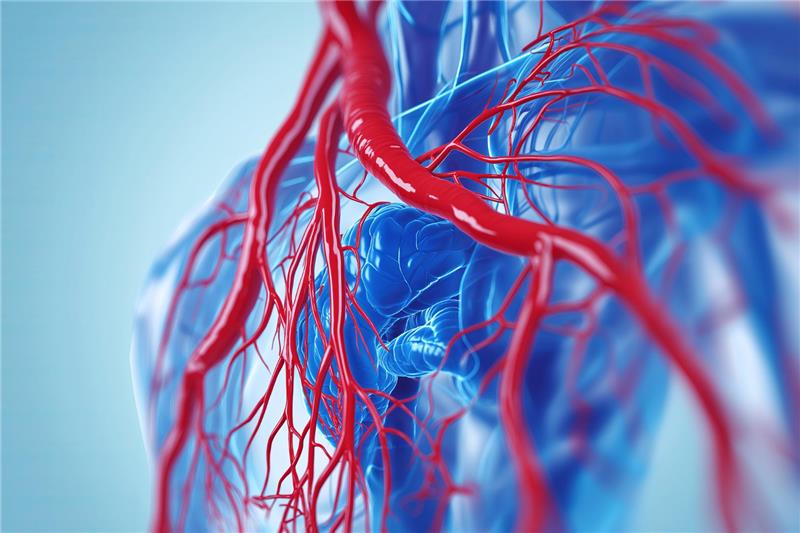
Heart failure is a chronic and progressive condition where the heart is unable to pump blood efficiently to meet the body's needs. Managing this condition requires a comprehensive approach that extends beyond symptomatic relief. One of the most effective strategies in the long-term management of heart failure is Optimal Medical Therapy (OMT). This term refers to a scientifically validated combination of medications and treatment strategies designed to improve survival, reduce hospitalizations, and enhance the quality of life for patients living with heart failure.
The Concept of OMT in Heart Failure
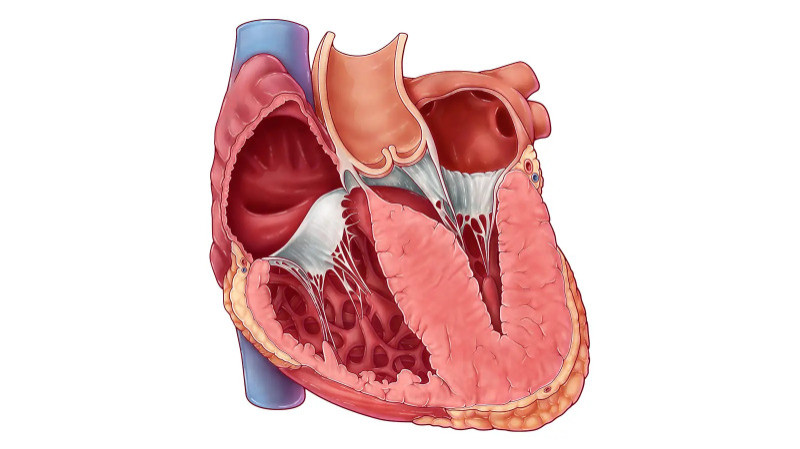
Optimal Medical Therapy is not a single medication or a fixed regimen. Instead, it refers to a personalized combination of medications proven through clinical trials to provide the best outcomes for patients with Heart Failure with Reduced Ejection Fraction (HFrEF) and, in some cases, Heart Failure with Preserved Ejection Fraction (HFpEF). The aim is to target the key mechanisms that drive heart failure progression—namely neurohormonal imbalance, fluid overload, and myocardial dysfunction.
This approach requires continuous monitoring, dose titration, and patient adherence. It is often adjusted based on disease progression, response to therapy, and the presence of comorbid conditions such as diabetes, hypertension, or chronic kidney disease.
Core Components of OMT
Optimal Medical Therapy typically includes several classes of medications that work in synergy. These include:
1. ACE Inhibitors or ARBs:
These drugs help relax blood vessels, lower blood pressure, and reduce the heart's workload. They also slow disease progression and reduce mortality.
2. Beta-Blockers:
Beta-blockers control heart rate and rhythm, improve cardiac function, and protect the heart from stress hormones. They have shown strong benefits in improving survival and reducing hospital readmissions.
3. Mineralocorticoid Receptor Antagonists (MRAs):
Drugs like spironolactone help counter the effects of aldosterone, which contributes to fluid retention and fibrosis. MRAs are especially beneficial in patients with severe symptoms.
4. SGLT2 Inhibitors:
Originally developed for diabetes, SGLT2 inhibitors like dapagliflozin and empagliflozin have shown remarkable benefits in heart failure patients—even those without diabetes—by reducing fluid overload and improving heart efficiency.
5. ARNI (Angiotensin Receptor-Neprilysin Inhibitor):
Sacubitril/valsartan has replaced ACE inhibitors in many patients due to its superior outcomes in reducing mortality and hospitalization rates.
6. Diuretics:
Though not proven to prolong survival, diuretics play a vital role in symptom management by helping the body eliminate excess fluid, relieving swelling and breathlessness.
7. Ivabradine (in select patients):
This medication is used to reduce heart rate in patients who are already on maximum beta-blockers but still have elevated heart rates.
Benefits of OMT
The primary advantage of Optimal Medical Therapy is its ability to modify the course of the disease. Clinical trials have demonstrated that patients on guideline-directed OMT experience fewer hospitalizations, lower rates of sudden cardiac death, and improved day-to-day functioning.
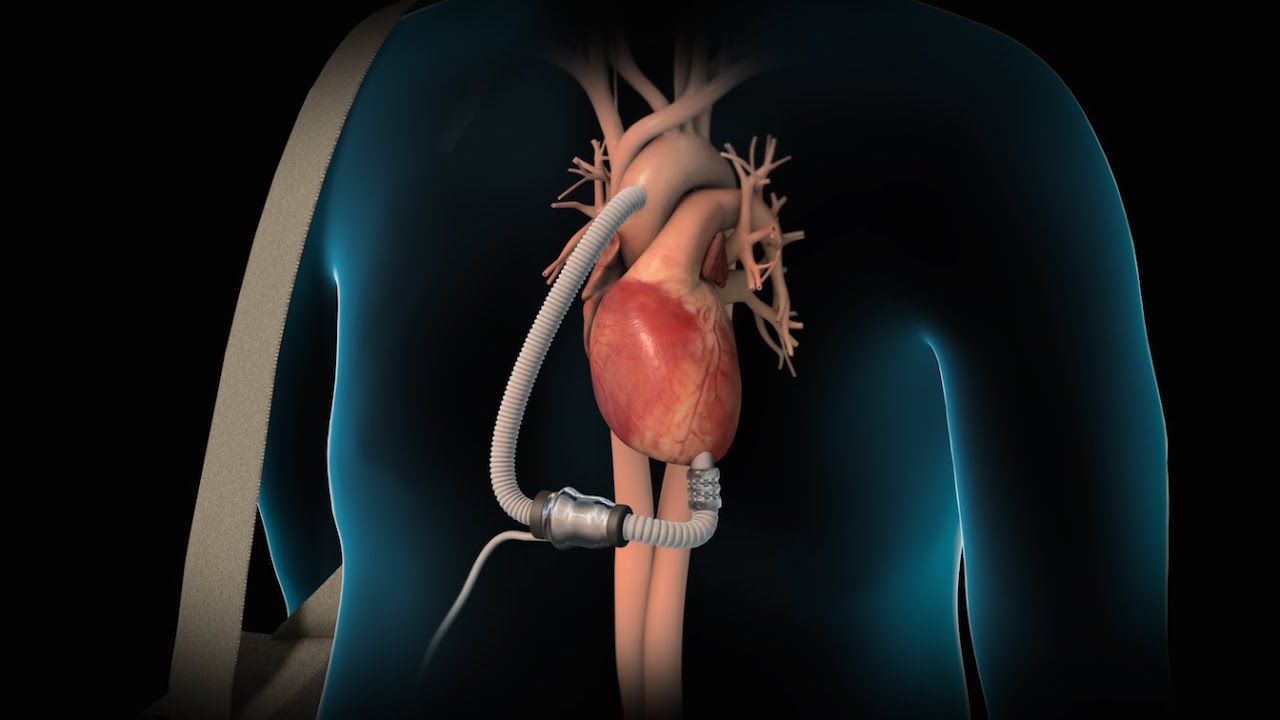
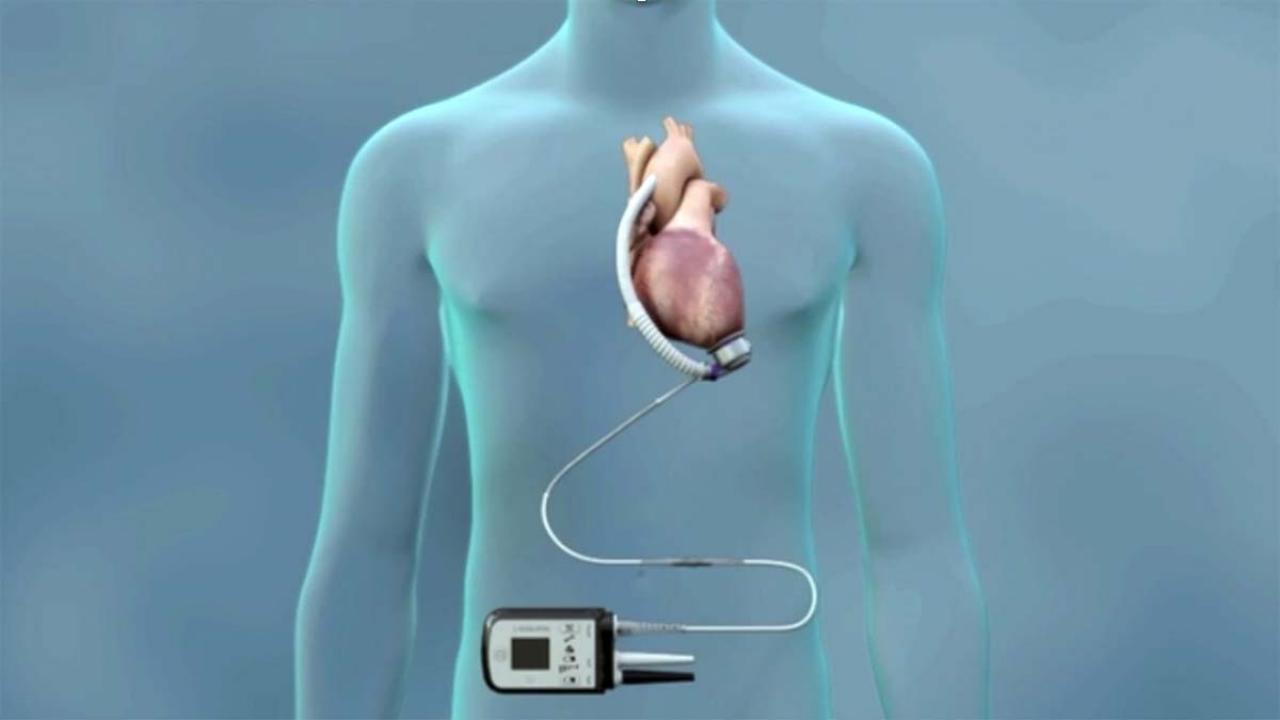
OMT also improves left ventricular function over time and reduces the burden on other organs such as the kidneys and liver, which are often affected in advanced stages of heart failure.
Tailoring Treatment for Individual Needs
No two patients with heart failure are exactly alike. Age, lifestyle, comorbidities, and the type of heart failure all play a role in determining the most suitable combination of therapies. OMT is often adjusted gradually, with careful attention to side effects and drug interactions.
For elderly patients or those with advanced kidney disease, for instance, dosages may need to be modified, and certain drugs may be substituted. This personalized approach is what makes OMT not only optimal but also adaptable and patient-centric.
Importance of Monitoring and Lifestyle Support
Medications alone are not enough. OMT is most effective when combined with regular monitoring, patient education, and lifestyle changes. Patients are encouraged to follow a low-sodium diet, engage in physician-approved physical activity, manage stress, and monitor their weight daily to detect early signs of fluid retention.
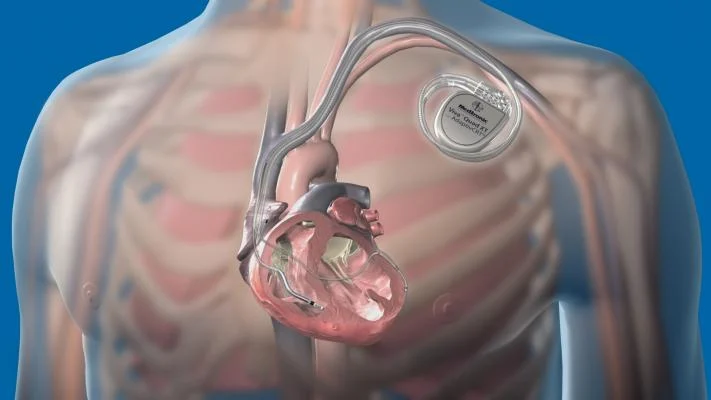
Frequent follow-ups, echocardiograms, and blood tests help ensure that the therapy remains optimal and effective over time. In some cases, cardiac rehabilitation programs are recommended to support physical recovery and improve mental well-being.
Future of OMT in Heart Failure
The concept of Optimal Medical Therapy continues to evolve with the development of new drugs and research findings. Advances in genetics, biomarkers, and remote monitoring tools may further personalize and refine OMT in the future. The ongoing expansion of SGLT2 inhibitors into broader heart failure populations is a recent example of how treatment guidelines are constantly being updated to reflect the best available evidence.
Conclusion
Optimal Medical Therapy represents a cornerstone in the management of heart failure, offering patients a scientifically proven path toward better health and longer life. Through a combination of carefully selected medications and regular monitoring, OMT helps control symptoms, slow disease progression, and enhance daily functioning. When implemented effectively, it shifts heart failure from a life-limiting condition to one that can be actively managed with confidence and care.