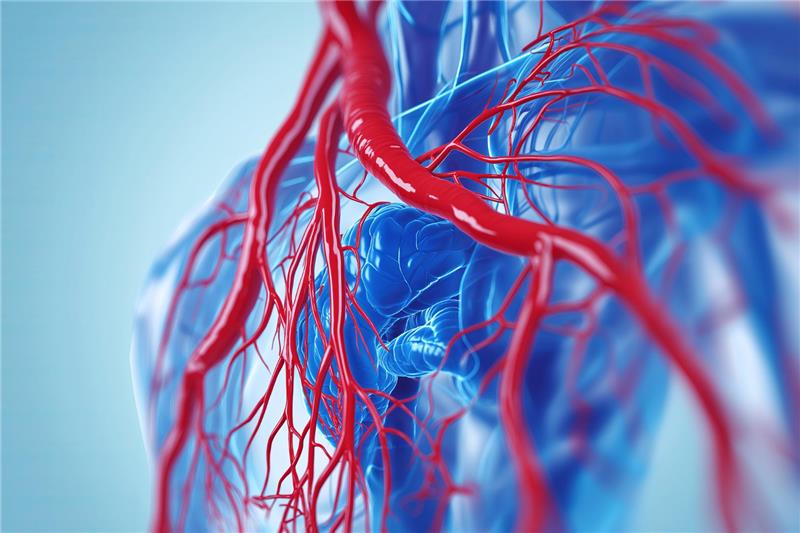
Heart failure occurs when the heart becomes unable to pump blood efficiently, resulting in reduced oxygen supply to the body. It’s not a single condition but a spectrum of disorders, each affecting the heart’s chambers differently. The most recognized classifications include left-sided, right-sided, and congestive heart failure. Differentiating among these helps tailor treatment and monitor symptoms effectively.
Left-Sided Heart Failure: The Common Form
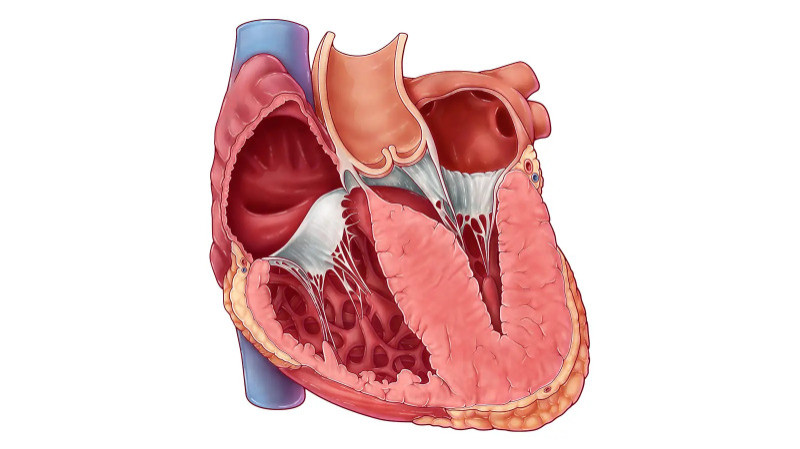
Left-sided heart failure is the most prevalent type and begins when the left ventricle weakens or becomes stiff. The left ventricle is responsible for pumping oxygenated blood to the entire body. When it underperforms, blood backs up into the lungs, causing pulmonary symptoms.
There are two variations: systolic heart failure, where the heart muscle cannot contract forcefully enough, and diastolic failure, where the ventricle is too stiff to fill adequately with blood. Symptoms typically include breathlessness, fatigue, and a chronic cough, especially noticeable during exertion or while lying flat. As the condition advances, other organs like the kidneys may suffer due to inadequate circulation.
Right-Sided Heart Failure: When Blood Backs Up in the Body
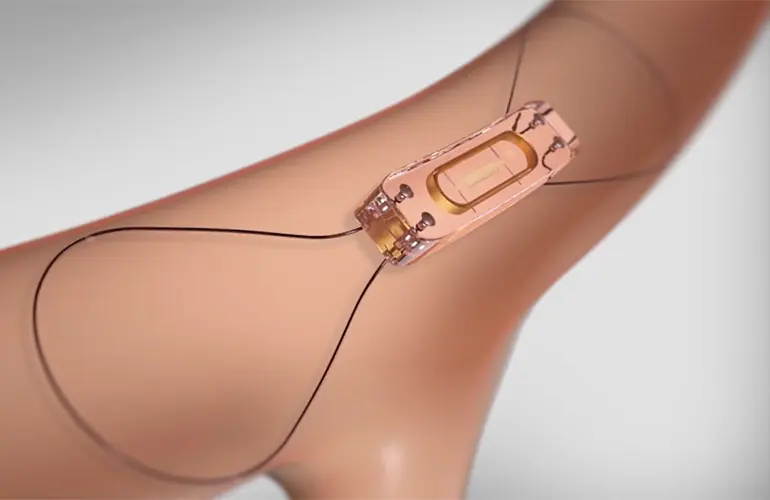
Right-sided heart failure impacts the right ventricle, which is tasked with sending deoxygenated blood to the lungs. When this chamber fails, blood backs up into veins, leading to visible swelling in the lower body, such as the legs, ankles, and abdomen.
This condition is often secondary to left-sided failure, as the strain from fluid buildup in the lungs forces the right side to work harder. It can also occur independently, triggered by lung-related disorders like pulmonary hypertension or chronic obstructive pulmonary disease (COPD). Signs include peripheral edema, sudden weight gain, and discomfort due to abdominal fluid retention.
Understanding Congestive Heart Failure
Congestive heart failure (CHF) represents a more advanced stage where both sides of the heart may be affected. The term “congestive” signifies fluid accumulation in tissues and organs due to inadequate circulation. It is not a separate category but rather a clinical manifestation of existing left or right heart dysfunction.
CHF can lead to symptoms such as difficulty breathing, wheezing, swelling in the limbs and abdomen, and increased nighttime urination. Over time, the body responds by holding on to salt and water, worsening fluid overload and leading to hospitalization if untreated.
Root Causes and Risk Triggers
Many factors can contribute to the onset of heart failure. Coronary artery disease, high blood pressure, valvular disorders, and a history of heart attacks are major culprits. Additionally, diabetes, obesity, excessive alcohol use, and certain infections raise the risk. Genetic conditions and inherited cardiomyopathies may also predispose younger individuals to early-onset heart failure.
Diagnosis: Identifying the Type of Failure
Diagnosing the specific type of heart failure involves a combination of imaging and lab tests. An echocardiogram helps assess heart muscle strength and chamber function. Other tests, such as chest X-rays, ECGs, and BNP blood levels, give further insight into fluid overload and electrical activity.
Distinguishing between left-sided, right-sided, or congestive failure allows clinicians to fine-tune therapy and address complications early on.
Treatment Strategies and Advanced Medications
Management focuses on symptom control, improving heart function, and preventing further damage. Medications form the backbone of therapy. Commonly used drugs include ACE inhibitors, beta-blockers, and diuretics to reduce fluid overload.
Mineralocorticoid receptor antagonists (MRAs), such as spironolactone or eplerenone, are now widely recommended, particularly for patients with reduced ejection fraction. These drugs help block harmful hormonal effects and reduce mortality.
For patients who continue to experience symptoms despite standard therapy, Vericiguat, a novel add-on drug, has shown promise. It works by enhancing nitric oxide signaling and improving vascular function. It’s typically prescribed in advanced cases where other treatments have not achieved full control.
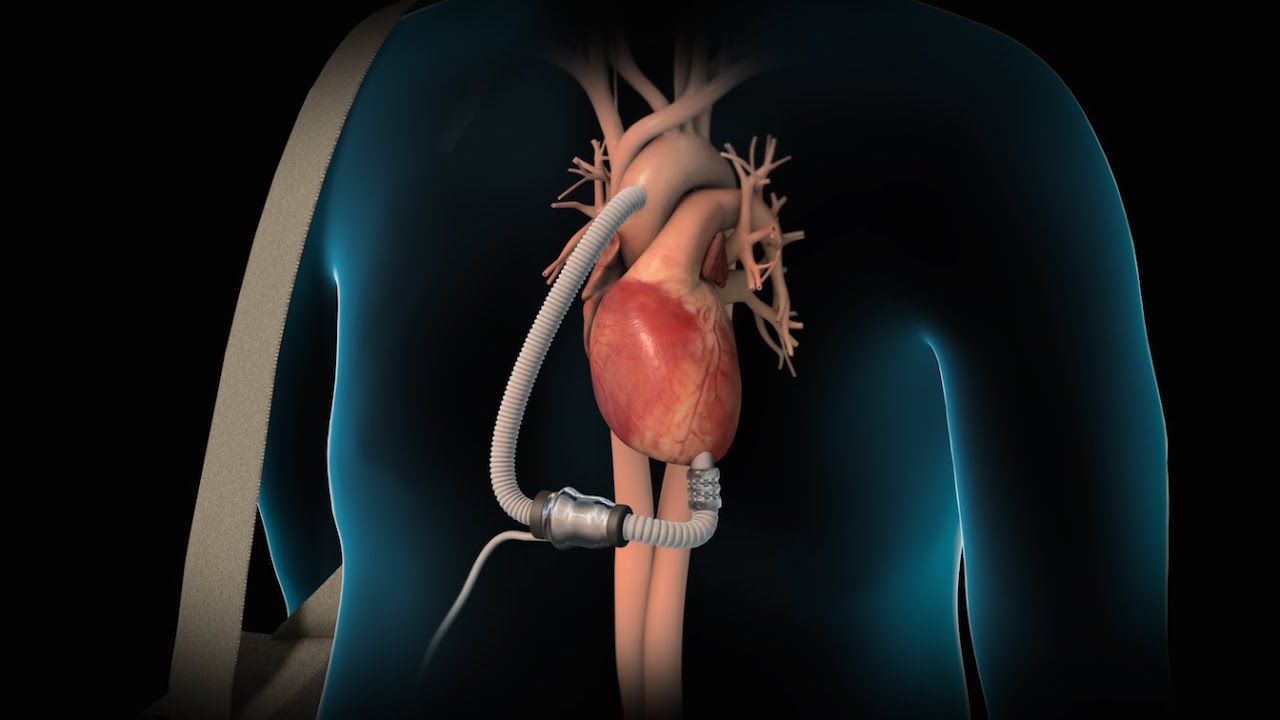
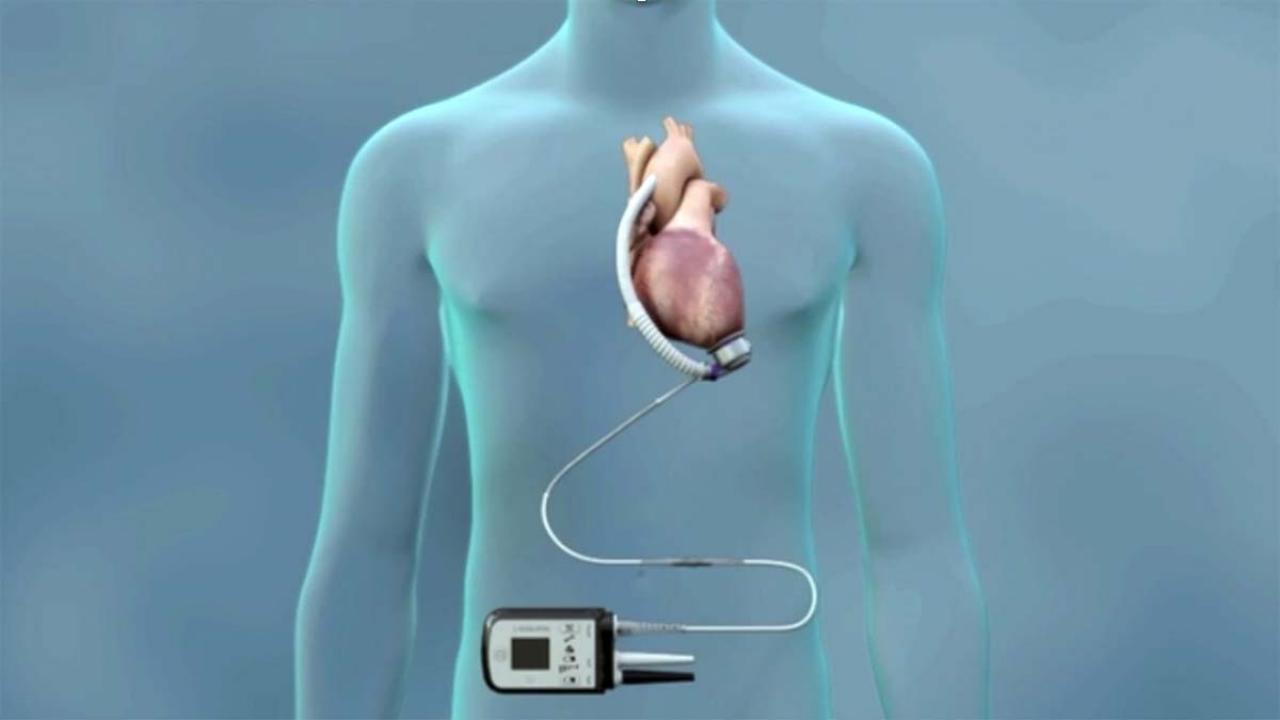
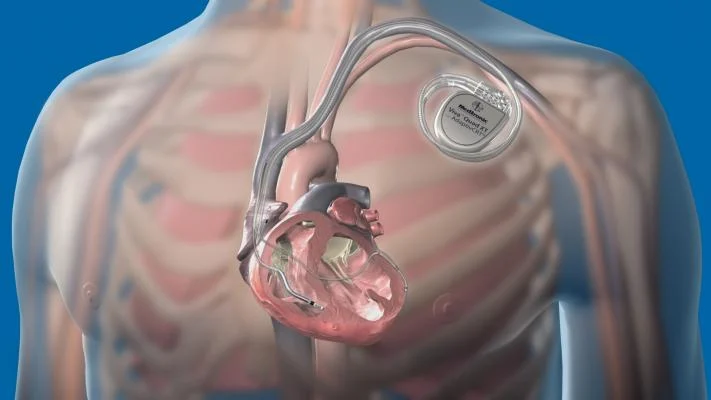
In severe heart failure, device-based therapies like implantable defibrillators, pacemakers, or surgical valve repair may be needed. Lifestyle changes—including sodium restriction, quitting smoking, moderate exercise, and fluid management—also play a critical role.
Conclusion
Heart failure is a multifaceted condition, presenting in various forms such as left-sided, right-sided, and congestive failure. Recognizing the unique signs of each type enables faster diagnosis and timely intervention. With a combination of modern medications, including MRAs and newer agents like Vericiguat, and supportive lifestyle changes, many individuals with heart failure can maintain a better quality of life and reduce hospitalizations. Early and personalized care is key to managing this challenging condition effectively.