Heart failure is a complex clinical condition where the heart fails to pump enough blood to meet the body's needs. With millions affected worldwide, it remains a leading cause of hospitalizations and mortality. Managing heart failure effectively requires not just medication but also constant monitoring of physiological parameters. This is where smart technologies like pressure sensor loops and advanced cardiac wearables have started playing a transformative role.
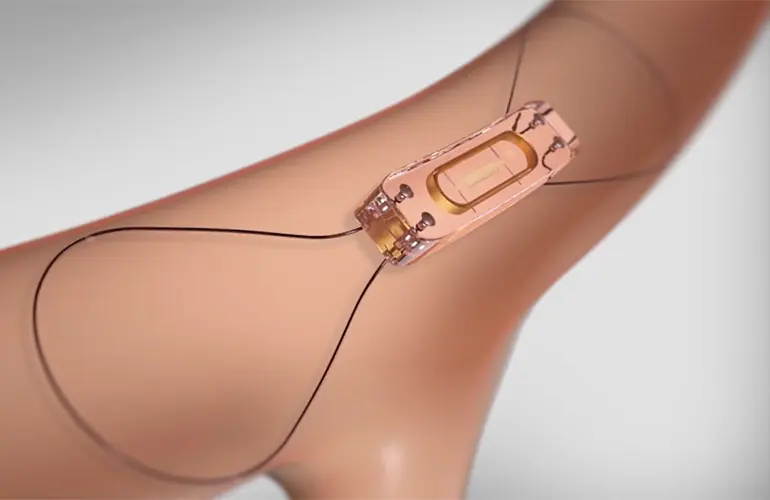
Understanding Pressure Sensor Loops
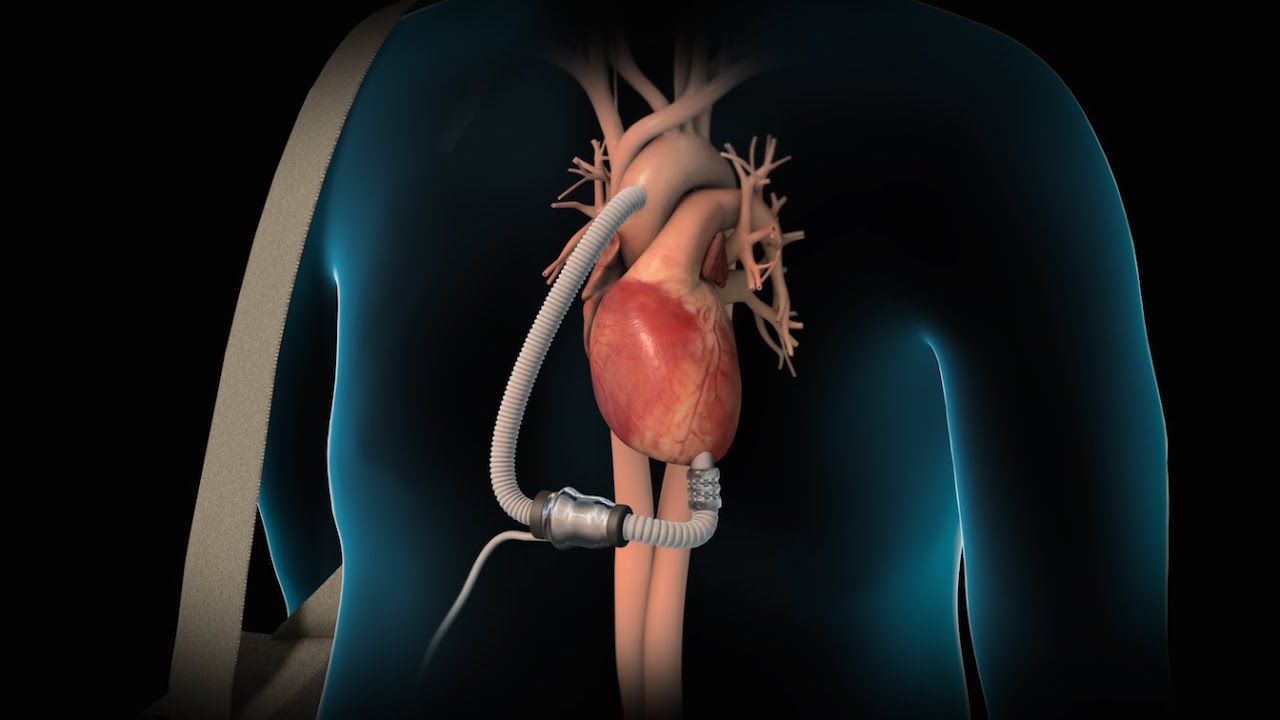
Pressure sensor loops are embedded devices designed to continuously monitor internal physiological pressures, particularly pulmonary artery pressure. These sensors are usually implanted inside the body and transmit real-time data to external devices or cloud-based systems. In heart failure management, pressure sensors help track fluid buildup in the lungs—a common sign of worsening heart function. By identifying such changes early, physicians can adjust treatment before symptoms become severe.
The most notable application of pressure sensor loops is in detecting increased pulmonary artery pressure, which typically rises days before a heart failure event. When used proactively, these devices help reduce hospital admissions and improve long-term outcomes. Data from the sensor loops can be integrated with patient management systems, allowing for a more personalized and precise therapeutic approach.
The Role of Cardiac Wearables
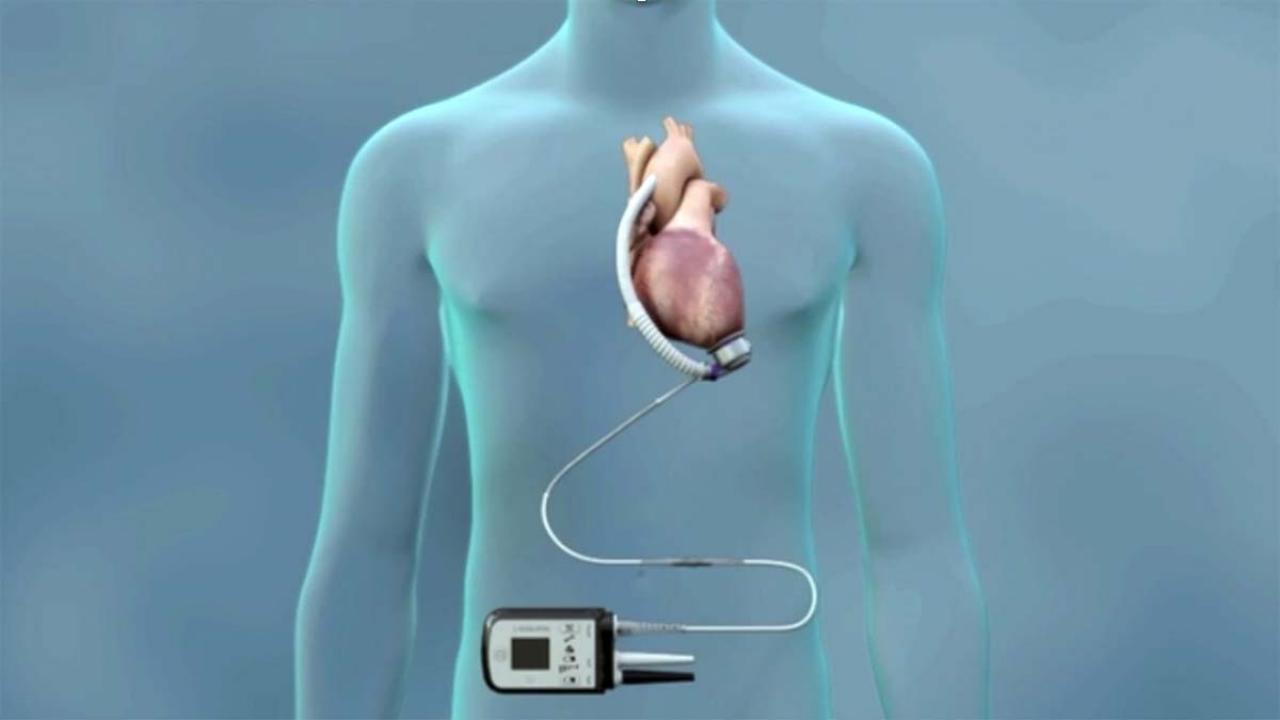
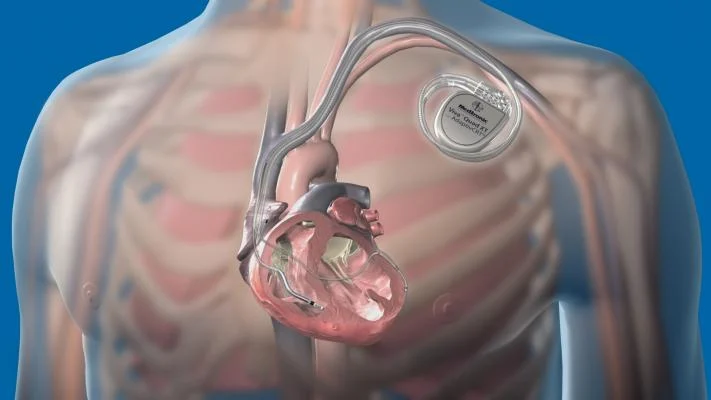
Cardiac wearables have evolved from basic fitness trackers to highly sophisticated medical-grade devices capable of monitoring heart rhythms, respiration, activity levels, and even body fluid levels. Devices such as cardiac resynchronization therapy (CRT), implantable cardioverter-defibrillators (ICDs), CRT-D (combination of CRT and defibrillator), and cardiac contractility modulation (CCM) systems are now widely used in heart failure treatment plans.
CRT and CRT-D Devices
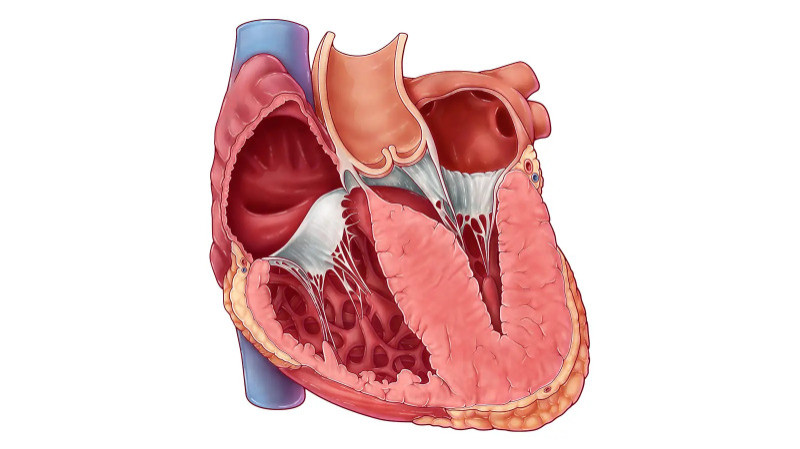
Cardiac Resynchronization Therapy (CRT) devices are used in patients with delayed heart muscle contractions. These devices improve coordination between the heart’s chambers, leading to more efficient blood pumping. CRT-D devices combine CRT with an implantable defibrillator. The defibrillator feature delivers a shock if life-threatening arrhythmias are detected, making CRT-D an essential tool for those at high risk of sudden cardiac death.
Both CRT and CRT-D devices have shown remarkable success in improving symptoms, reducing hospitalizations, and extending survival in patients with moderate to severe heart failure. These wearables are usually implanted under the skin and continuously monitor the heart’s electrical activity, adjusting pacing as needed.
Implantable Cardioverter-Defibrillators (ICDs)
ICDs are designed to detect and correct abnormal heart rhythms (arrhythmias). For heart failure patients prone to ventricular tachycardia or fibrillation, ICDs act as a safety net. These devices not only monitor heart rhythm but also intervene by delivering shocks to restore normalcy. The use of ICDs in appropriate heart failure populations has led to a significant reduction in sudden cardiac deaths.
Cardiac Contractility Modulation (CCM)
CCM devices are relatively newer in the field of heart failure therapy. Unlike CRT, which targets electrical synchrony, CCM focuses on improving the heart’s pumping strength by delivering non-excitatory electrical signals during the absolute refractory period of the cardiac cycle. These signals enhance calcium handling in cardiac cells, improving contractility and cardiac output. CCM therapy is especially beneficial for patients who are not eligible for CRT due to normal QRS duration.
Medications and the Role of Add-On Therapies
In addition to wearable technologies, pharmacological management remains the cornerstone of heart failure treatment. Medications like ACE inhibitors, beta-blockers, and mineralocorticoid receptor antagonists (MRAs) are foundational in therapy. MRAs such as spironolactone and eplerenone reduce sodium retention, control blood pressure, and prevent fibrosis, all of which are key in managing heart failure progression.
Newer medications like Vericiguat, a soluble guanylate cyclase stimulator, are now being used as add-on drugs in patients with worsening heart failure despite standard therapy. Vericiguat improves vasodilation and reduces heart strain, thus offering additional support alongside device-based management strategies.
Integration of Digital Health Platforms
The real power of pressure sensor loops and cardiac wearables lies in their integration with digital health ecosystems. Remote monitoring platforms allow healthcare providers to access continuous patient data, interpret trends, and respond promptly. Artificial intelligence and machine learning tools are increasingly being used to analyze this data, predict exacerbations, and provide decision support to clinicians.
Furthermore, patients equipped with mobile apps linked to their devices gain greater awareness of their condition, leading to better medication adherence and lifestyle changes. The combination of wearable technology with smart health platforms represents a holistic approach to heart failure care, transitioning from reactive to preventive management.
Challenges and Future Directions
Despite the advantages, challenges remain in widespread adoption. Cost, patient compliance, and access to specialized care are significant barriers, especially in resource-limited settings. There is also the need for more longitudinal data to understand the long-term benefits of these technologies across various subgroups of heart failure patients.
The future, however, looks promising. As technology continues to evolve, smaller, more efficient, and cost-effective devices are being developed. Combined with advances in wireless connectivity and AI, these innovations will likely redefine how heart failure is diagnosed, monitored, and treated in the coming years.
Conclusion
Smart pressure sensor loops and advanced cardiac wearables such as CRT, CRT-D, ICDs, and CCM systems are revolutionizing heart failure management. These technologies offer real-time monitoring, early detection of complications, and improved therapeutic outcomes. When integrated with medications like MRAs and Vericiguat, and supported by digital platforms, they represent the future of proactive and personalized cardiac care.