Heart failure refers to a chronic condition in which the heart loses some of its ability to pump blood efficiently. Despite the term “failure,” it doesn’t mean the heart has stopped working outright. Instead, it indicates that the organ has become too weak or too stiff to meet the body’s demands. Over time, this condition can significantly affect quality of life—but with proper diagnosis and management, many people continue to live well
What Leads to Heart Failure?
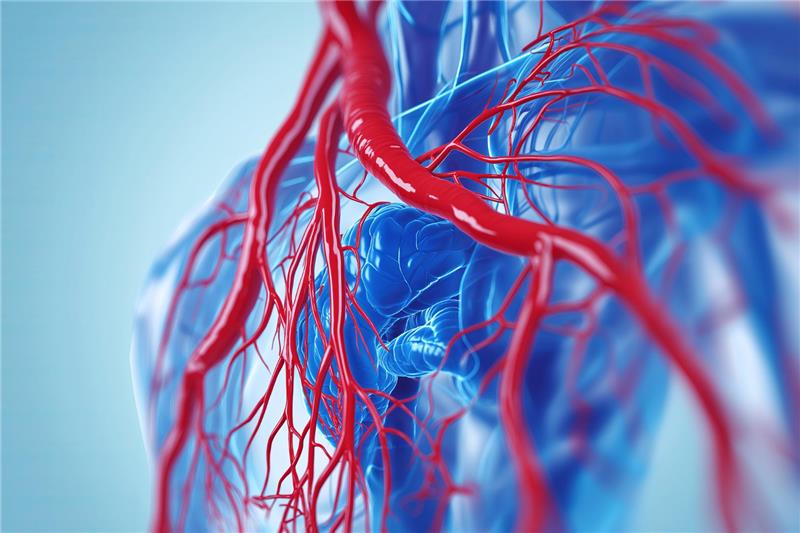
Heart failure typically develops gradually, as other health issues slowly weaken the heart. A leading cause is coronary artery disease, where plaque builds up in arteries, reducing blood flow to the heart muscle. This can starve the heart of oxygen and lead to cells dying, gradually weakening the heart’s performance.
Uncontrolled high blood pressure also places extra strain on the heart. Over years, this pressure forces the heart muscle to thicken, making it less elastic and less efficient at pumping blood. Previous heart attacks or damage to the heart muscle contribute further by creating scar tissue that limits healthy contraction.
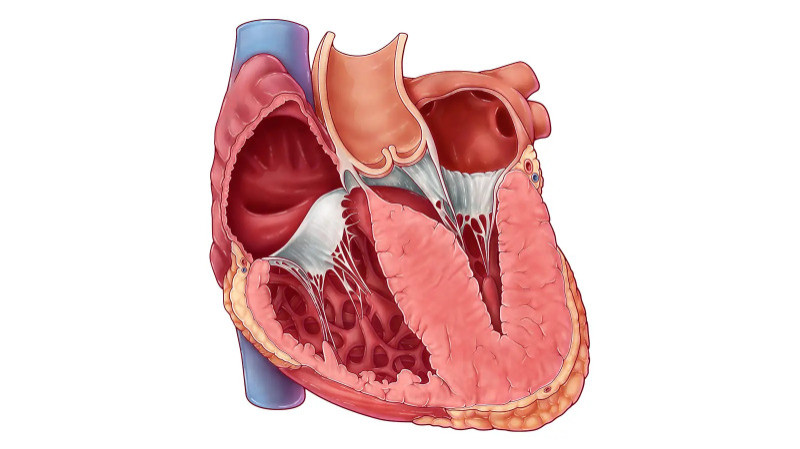
In addition, conditions like cardiomyopathy—where the heart muscle becomes diseased—or valve dysfunction, where heart valves fail to open or close properly, can pave the way to heart failure. Factors such as obesity, diabetes, thyroid disorders, heavy alcohol use, and certain medications or infections also increase risk by affecting heart structure or function.
Recognizable Symptoms of a Failing Heart
Symptoms of heart failure often begin subtly and may worsen over time. Shortness of breath is one of the first signs, appearing during activity, when lying down, or even at rest in advanced cases. This occurs because fluid can back up into the lungs when the heart is unable to pump effectively.
Other common signs include fatigue, as insufficient blood flow deprives muscles and organs of energy, and swelling (edema) in the legs, ankles, or abdomen due to fluid accumulation. Patients might also experience persistent cough, wheezing—which may produce pink or white phlegm—rapid or irregular heartbeat, lightheadedness, or sudden weight gain from retained fluid.
These symptoms typically worsen gradually, making daily tasks like climbing stairs or carrying groceries increasingly difficult.
Understanding the Four Stages
Doctors classify heart failure into stages from A to D, based on symptoms and heart function tests. These stages guide treatment decisions:
Stage A: No symptoms or structural heart issues—but risk factors such as hypertension, diabetes, or family history are present.
Stage B: Structural changes in the heart—such as thinning, thickening, or scarring—but no noticeable symptoms.
Stage C: Structural changes with symptoms like fatigue, breathlessness, or swelling. At this stage, treatment aims to reduce symptoms and improve quality of life.
Stage D: Advanced phase requiring specialized interventions. Symptoms persist despite standard therapies, and options may include surgical procedures or advanced devices.
How Is Heart Failure Diagnosed?
To confirm heart failure, doctors perform a thorough clinical evaluation. This includes listening for lung congestion and irregular heart rhythms and checking for swelling in the legs or abdomen. Blood tests measure markers like brain natriuretic peptide (BNP), which rise when the heart is overloaded.
Imaging techniques such as echocardiography provide a visual assessment of pumping ability, chamber sizes, and valve health. An electrocardiogram (ECG) identifies arrhythmias or past heart muscle damage, while chest X-rays reveal lung congestion and heart enlargement. More advanced testing like cardiac MRI, CT scans, or stress tests may be used in specific cases.
Strategies for Treatment and Management
Although heart failure cannot be reversed, progression can be slowed, and symptoms relieved. Treatment typically combines lifestyle changes, medications, and, in some cases, medical devices or procedures.
Lifestyle adjustments are foundational. Reducing salt intake, losing excess weight, quitting smoking, limiting alcohol, and engaging in moderate exercise—all under medical supervision—can significantly ease the heart’s workload.
Common therapies include:
ACE inhibitors or ARBs to help the heart pump more efficiently.
Beta-blockers to manage heart rhythm and reduce oxygen demand.
Diuretics to relieve fluid buildup.
Aldosterone antagonists to reduce strain on the heart and prevent hospitalization.
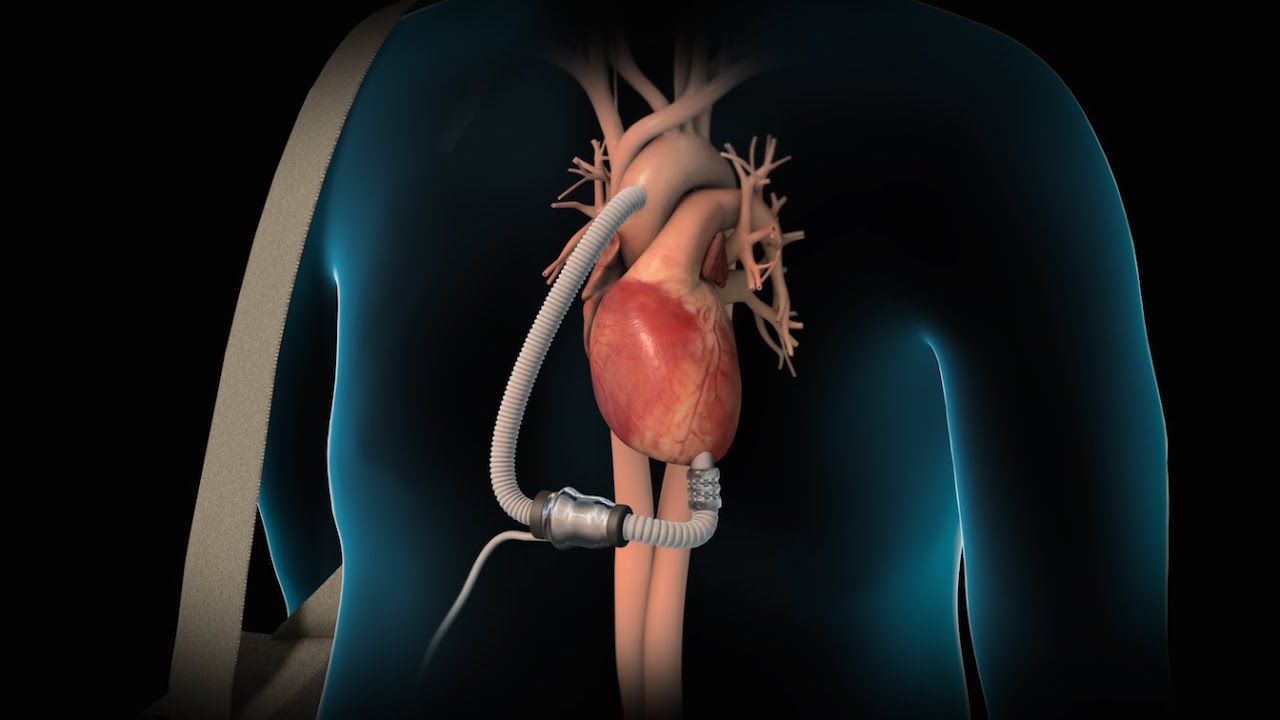
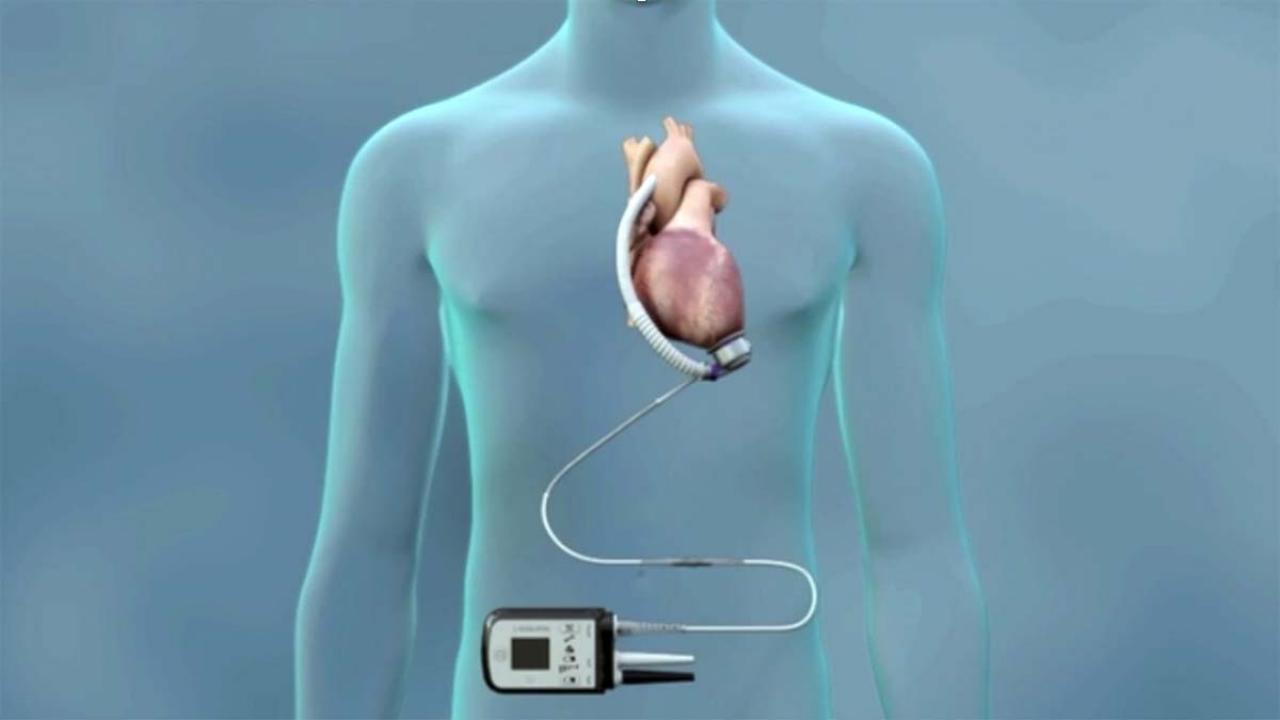
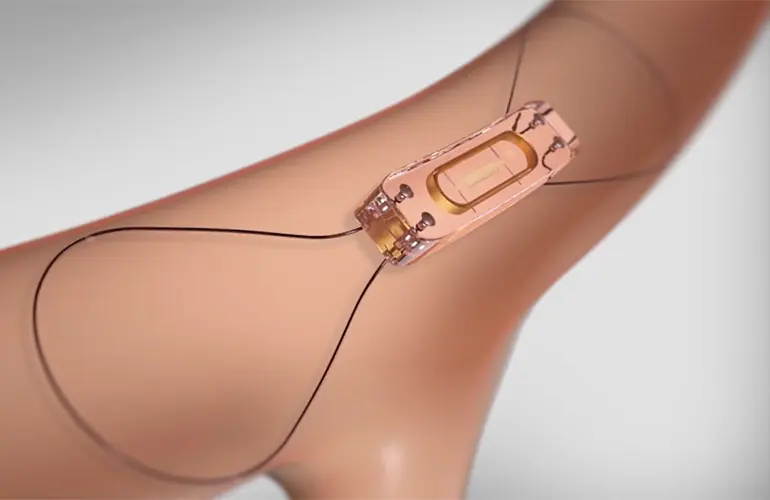
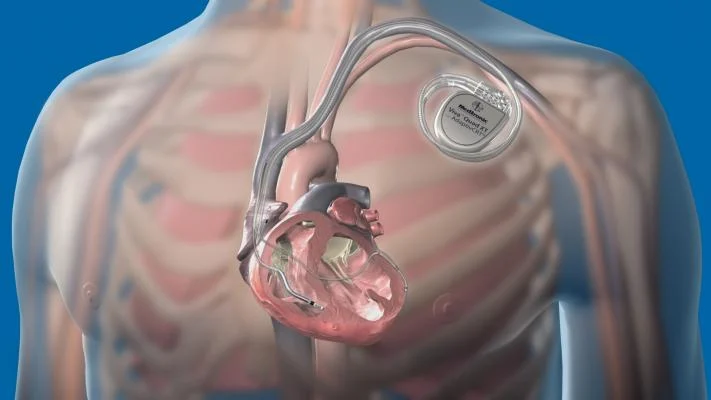
Device interventions such as pacemakers, implantable defibrillators (ICDs), or left ventricular assist devices (LVADs) may be recommended in advanced cases to stabilize the heartbeat or support circulation. In some scenarios, heart transplant remains an option.
Patient education, emotional support, and regular monitoring are vital. Clinics often offer support groups to help patients and caregivers navigate challenges and celebrate progress.
Living Well With Heart Failure
Managing heart failure effectively involves ongoing attention. Regular follow-up visits monitor symptoms, medication effects, and lifestyle habits. Blood work, imaging, and heart function assessments help doctors adjust treatment as needed.
Patients are advised to watch for warning signs like sudden increases in weight, intensified shortness of breath, or worsening fatigue. Prompt medical attention for these changes can prevent hospitalization or disease worsening.
Family involvement, emotional support, and access to rehabilitation or counseling services are key in helping patients regain confidence and maintain independence.
Conclusion
Heart failure is a serious but manageable condition. Although its impact on daily life can be profound, thoughtful treatment and lifestyle modifications can make a significant difference. By recognizing early warning signs, understanding the staging system, and committing to a personalized care plan, patients can slow disease progression and improve both longevity and quality of life.
With advances in medicine and ongoing support from healthcare teams, individuals living with heart failure can continue to live purposeful, fulfilling lives—one step at a time.