Heart failure is a chronic, progressive condition where the heart becomes too weak to pump blood efficiently. In its early stages, medications, lifestyle adjustments, and devices like pacemakers can manage symptoms and slow progression. But when these options no longer offer relief, and the heart's function continues to decline, the condition enters its most advanced phase—end-stage heart failure. At this critical point, a heart transplant is often the only option left to restore life and function.
What Happens in End-Stage Heart Failure
As heart failure advances, the heart muscles weaken, causing a drop in the amount of blood pumped to vital organs. This can lead to extreme fatigue, shortness of breath even at rest, frequent fluid retention, and repeated hospitalizations. For patients who no longer respond to high doses of medication or implanted devices, a transplant becomes a consideration. End-stage heart failure drastically reduces quality of life and life expectancy, and the only potentially life-saving treatment is replacing the damaged heart.
What Is a Heart Transplant?
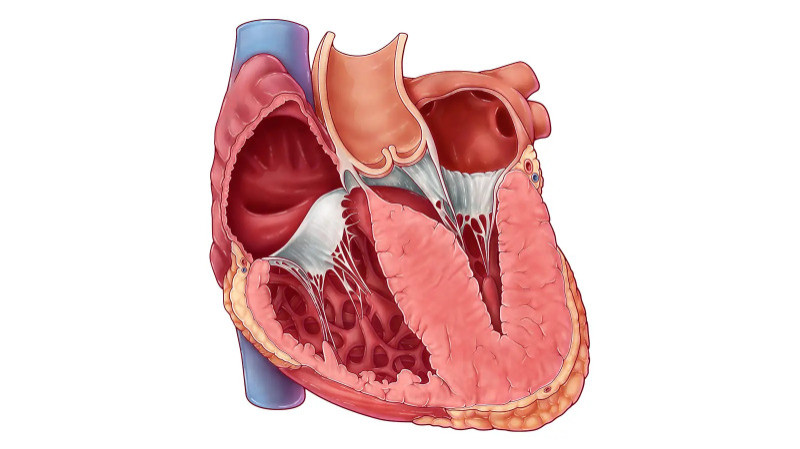
A heart transplant is a complex surgical procedure in which a diseased or failing heart is replaced with a healthy one from a deceased donor. Donors are usually individuals who have suffered irreversible brain death but whose other organs are still functioning. The surgery is performed only after careful evaluation of the recipient’s physical, emotional, and psychological readiness.
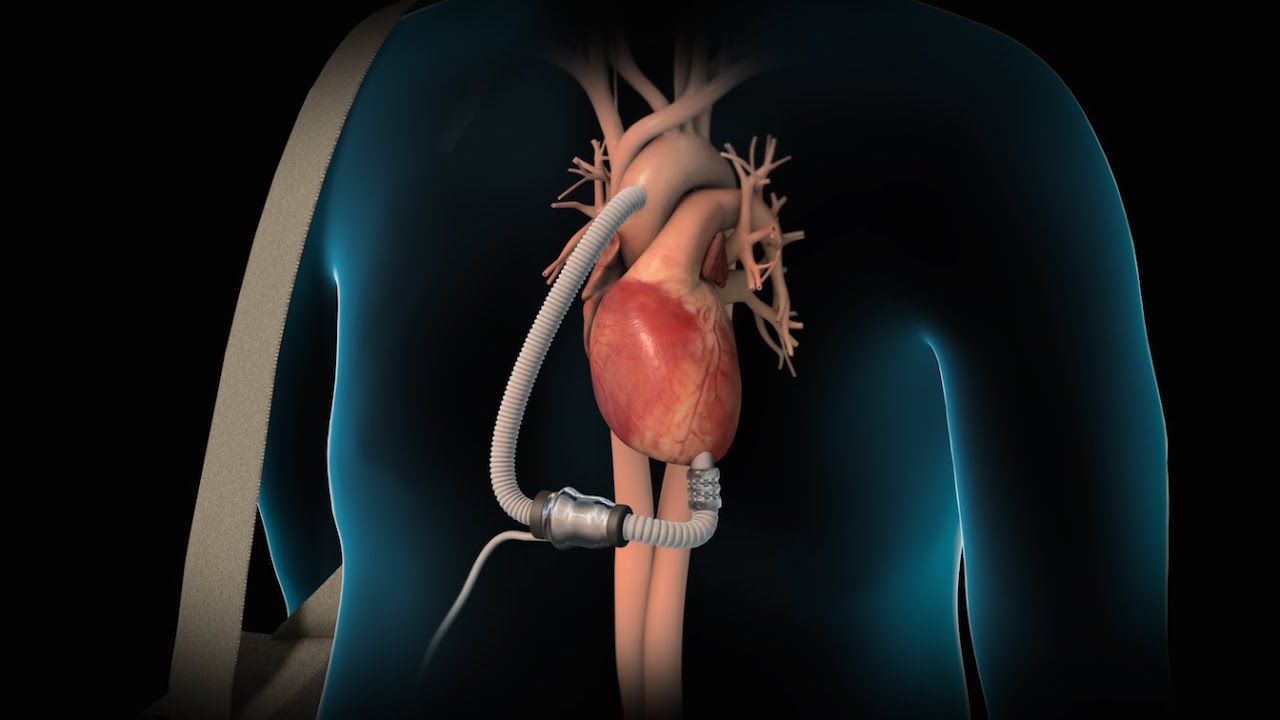
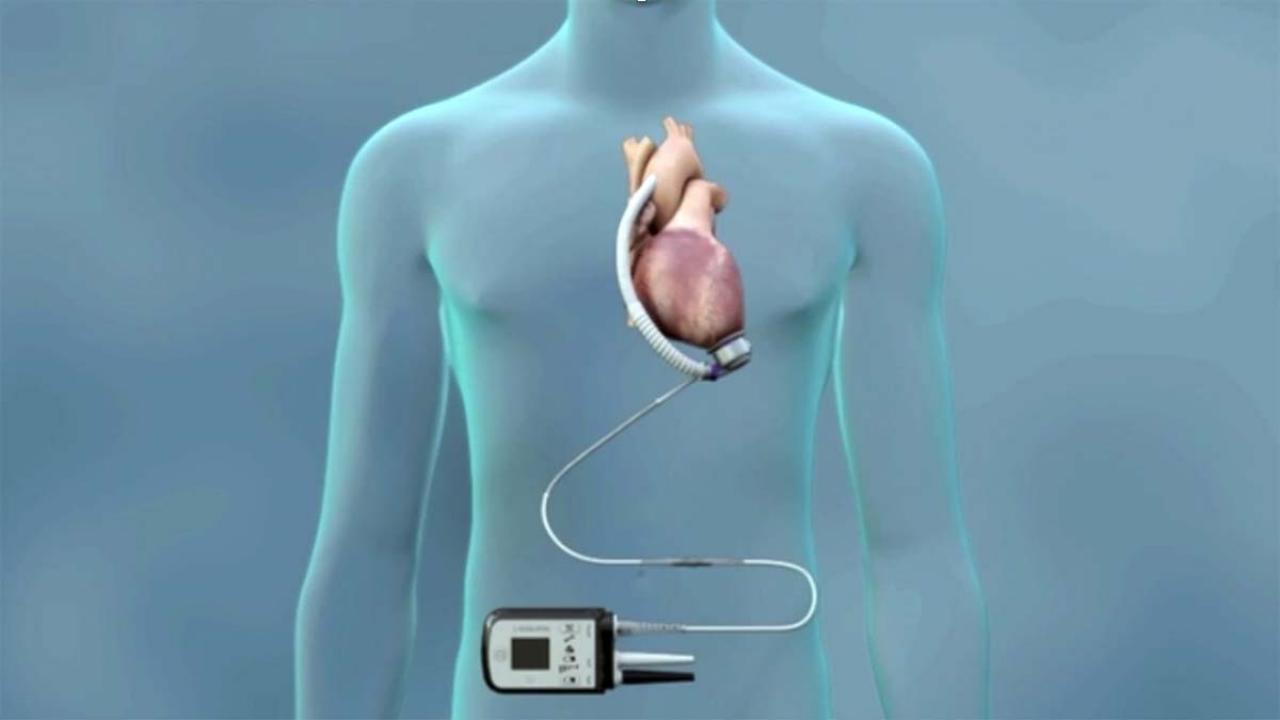
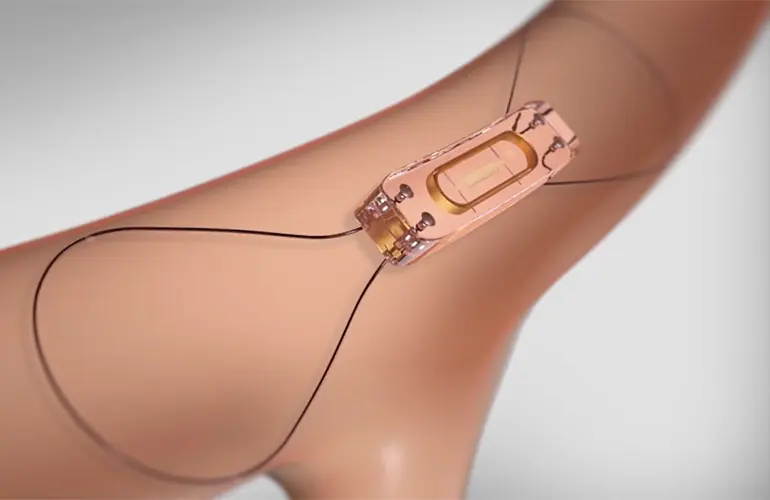
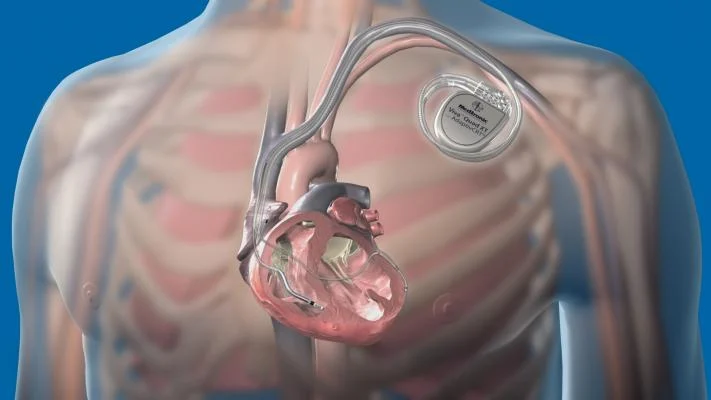
Due to the limited availability of donor hearts, patients are added to a national waiting list and prioritized based on factors such as blood type, medical urgency, body size, and overall health. While waiting, patients are monitored closely and may require temporary support devices like LVADs to maintain heart function.
Who Is a Candidate for Heart Transplantation?
Not all patients with heart failure qualify for a transplant. Candidates must meet specific criteria. They must be in end-stage heart failure, have exhausted all other treatments, and be otherwise healthy enough to undergo surgery and manage long-term care. Conditions such as severe lung, liver, or kidney disease, uncontrolled infections, or ongoing substance abuse can disqualify a patient.
A multidisciplinary team of cardiologists, surgeons, psychologists, and social workers assess whether a transplant will truly benefit the patient and if they can manage post-transplant demands like medication adherence and lifestyle changes.
The Transplant Surgery Process
Once a donor heart becomes available and a match is confirmed, the patient is quickly prepared for surgery. The operation typically lasts several hours. During the procedure, the chest is opened, and the diseased heart is removed. The donor heart is then placed and connected to the main blood vessels. A heart-lung machine keeps blood and oxygen flowing through the body while the heart is being replaced.
Once the new heart is in position and beating effectively, the machine is removed. The patient is then moved to an intensive care unit for close monitoring over the next few days. Recovery in the hospital can take a few weeks, depending on the patient’s overall condition and response.
Life After a Heart Transplant
Post-transplant life involves a major adjustment. The most crucial part of recovery is preventing rejection. Since the body recognizes the donor heart as foreign, it may attempt to attack it. To prevent this, patients must take immunosuppressant medications for the rest of their lives. These medications lower the immune system’s response but can also increase the risk of infections and other complications.
Regular follow-up appointments, heart biopsies, blood tests, and imaging help ensure the new heart is functioning well. Patients are also advised to adopt a healthy lifestyle, including a balanced diet, regular physical activity, avoiding smoking and alcohol, and managing stress. With consistent care, many transplant recipients are able to return to work, travel, and enjoy everyday activities.
Risks and Complications
While heart transplants can be life-saving, they are not without risks. Rejection is one of the most common concerns, especially within the first year. Other complications include infections due to immune suppression, coronary artery disease in the transplanted heart, kidney problems, and an increased risk of certain cancers over time.
Despite these risks, advances in surgical techniques and post-operative care have significantly improved long-term outcomes. Many recipients live for 10 years or more after their transplant, with some surviving for two decades or longer.
Looking Ahead: The Future of Heart Transplants
Medical research continues to explore new frontiers to make heart transplants more successful and accessible. Artificial hearts, stem cell therapy, and improved organ preservation techniques are some of the areas being developed. These innovations could potentially reduce the need for donor hearts and improve survival rates in the future.
Efforts are also being made to raise awareness about organ donation. Increasing the donor pool can help save more lives and reduce waiting times for those in need of a transplant.
Conclusion
A heart transplant is more than a surgical procedure—it is often the final hope for those battling end-stage heart failure. While it comes with challenges, it also provides the possibility of a longer, healthier life. With proper post-operative care and a commitment to maintaining health, transplant recipients can regain independence and significantly improve their quality of life. The journey may be complex, but for many, it leads to a renewed sense of purpose and a second chance at life.