Heart failure is a progressive condition that impairs the heart’s ability to pump blood efficiently. While lifestyle changes and medications are the first line of treatment, some individuals continue to experience worsening symptoms. In such cases, advanced therapies are considered. One of the most impactful interventions is device therapy, which uses implanted medical devices to improve heart function and prevent complications.
The Purpose of Device-Based Interventions
The goal of device therapy is not only to manage symptoms but also to reduce the risk of sudden cardiac events and hospitalizations. It offers a lifeline to patients whose hearts are structurally or electrically impaired, even after receiving optimal medical treatment. The selection of the appropriate device depends on the type of heart failure and the patient’s overall clinical status.
Identifying Candidates for Device Therapy
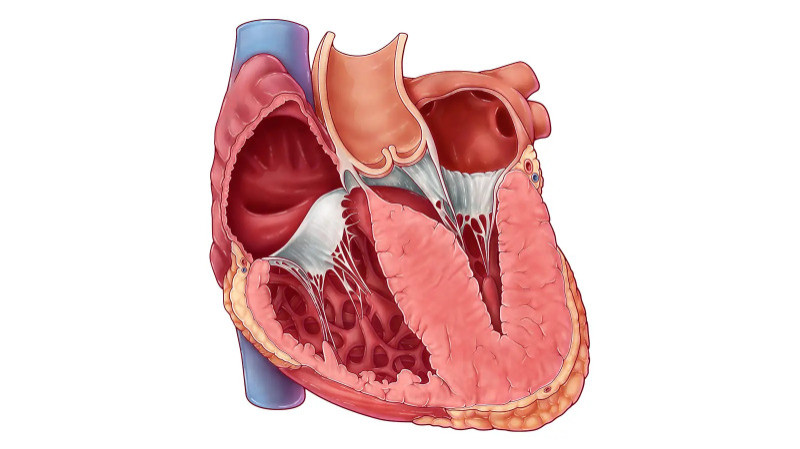
Not all individuals with heart failure require devices. Physicians follow strict clinical guidelines before recommending such treatment. Patients are usually evaluated on the basis of their left ventricular ejection fraction (LVEF)—a key measure of how well the heart is pumping. A reduced LVEF, typically below 35%, suggests that the heart is failing to circulate blood effectively.
Additionally, individuals experiencing persistent symptoms despite taking maximum doses of heart failure medications are likely candidates. Electrical abnormalities in heart rhythms, such as prolonged QRS intervals or arrhythmias, are also strong indicators for device intervention.
Common Types of Devices in Use
Several devices are commonly used, each serving a different purpose based on the underlying cardiac condition.
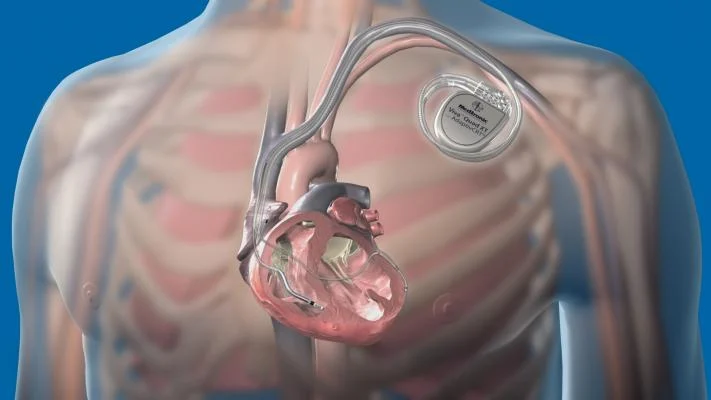
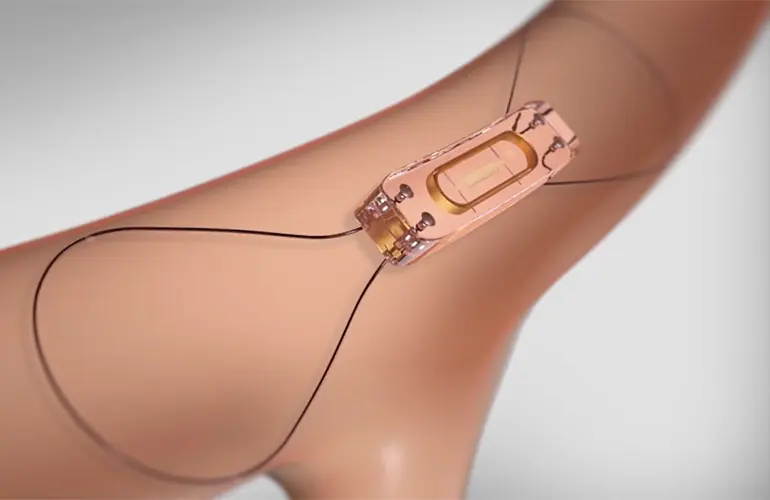
Implantable Cardioverter Defibrillators (ICDs) are inserted into patients at risk of sudden cardiac arrest. These devices monitor heart rhythms continuously and deliver a life-saving shock if a dangerous arrhythmia is detected.
Cardiac Resynchronization Therapy (CRT) involves a specialized pacemaker that coordinates the contractions of the heart’s left and right ventricles. It is especially effective in patients with delayed or uncoordinated heartbeats, improving both function and symptoms.
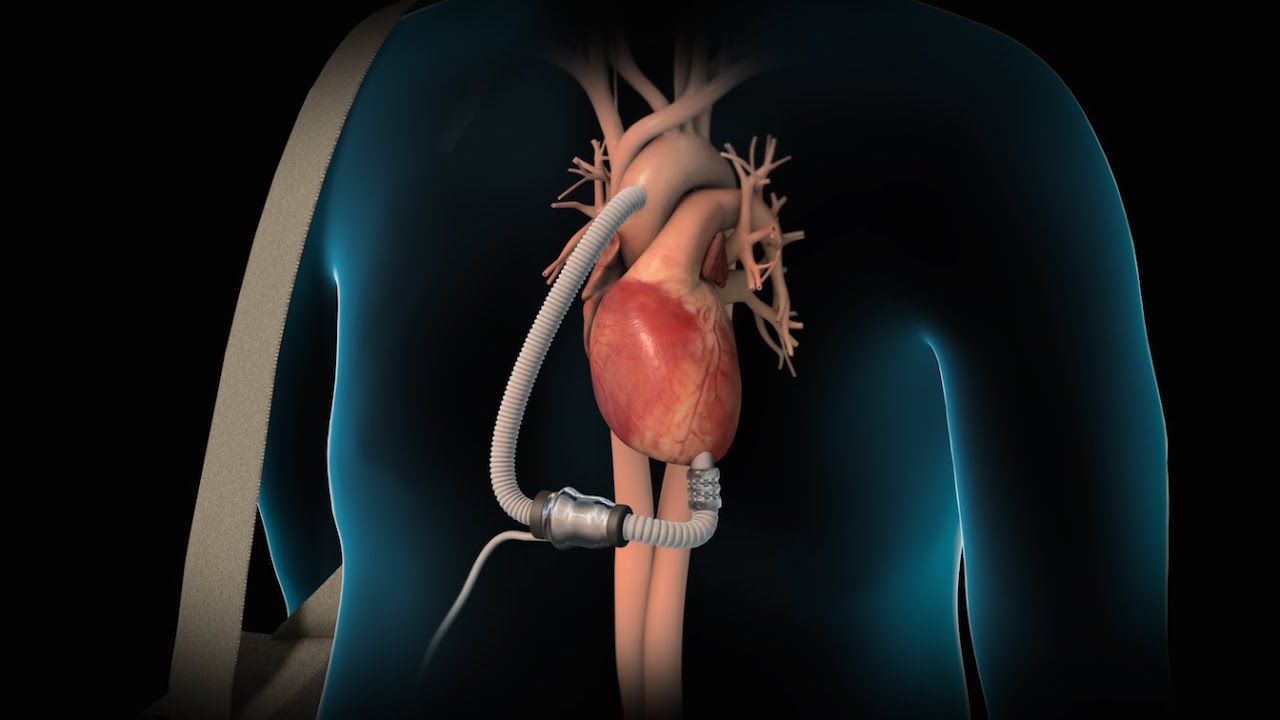
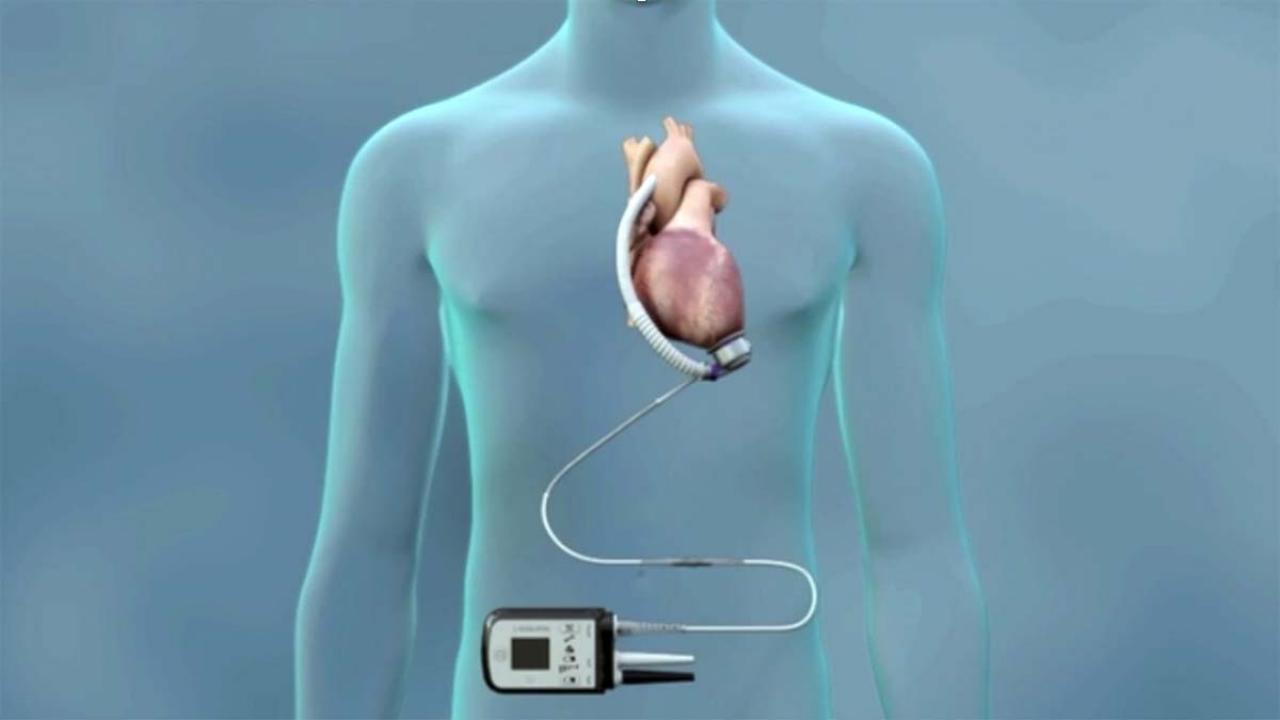
Ventricular Assist Devices (VADs) are mechanical pumps that support heart function in patients with advanced or end-stage heart failure. These devices are often used as a bridge to transplant or as a long-term solution when transplantation is not possible.
When Is the Right Time to Consider a Device?
Device therapy is considered when patients meet the following criteria:
Continued symptoms despite optimal drug therapy
Left ventricular ejection fraction of 35% or lower
History or risk of life-threatening arrhythmias
Evidence of conduction abnormalities like left bundle branch block
Repeated hospitalizations due to heart failure
Patients with advanced heart failure who are ineligible for heart transplant may benefit significantly from long-term mechanical support with VADs.
Impact and Benefits of Device Therapy
For eligible patients, device therapy can be life-changing. These devices not only help improve heart function but also reduce the likelihood of sudden cardiac death and emergency admissions. Many patients report better energy levels, improved breathing, and an overall enhanced quality of life after device implantation.
Moreover, devices like CRT can help the heart muscle recover over time by restoring synchronized contractions, a process known as cardiac remodeling. This long-term improvement often reduces the need for further interventions.
Ongoing Monitoring and Care
After implantation, regular follow-ups are essential to ensure the devices function correctly. Patients are typically monitored through in-person check-ups and, in many cases, through remote telemetry. Adjustments may be needed over time to match the patient’s evolving health needs.
Lifestyle guidance also plays a role in ensuring long-term success. Patients are advised to avoid high electromagnetic fields and report any unusual symptoms immediately.
Conclusion
Device therapy represents a significant advancement in the treatment of heart failure. For patients who do not respond adequately to medications, these devices provide critical support and may even extend life expectancy. By carefully evaluating the severity and progression of heart failure, specialists can determine the most appropriate time to introduce device-based solutions, leading to better outcomes and an improved quality of life.